A Chance to Modernize Health Care behind Bars, Section 1115 Medicaid Inmate Exclusion Waivers | NEJM, Brendan Saloner, Ph.D. California and Washington are the first states to receive waivers from the Centers for Medicare and Medicaid Services (CMS) regarding the Medicaid Inmate Exclusion Policy. The policy generally prohibits Medicaid from paying for health care for people who are incarcerated. That being said, ~2 million Americans were incarcerated on any given day in 2020 and 2021.1 Disproportionately, people who are incarcerated are poor and members of a marginalized racial or of ethnic groups. They typically have elevated rates of mental illness, substance use disorders, and other chronic diseases.1 Engaging members of this population in
Topics:
Bill Haskell considers the following as important: Education, politics, Prison Healthcare
This could be interesting, too:
Robert Skidelsky writes Lord Skidelsky to ask His Majesty’s Government what is their policy with regard to the Ukraine war following the new policy of the government of the United States of America.
Joel Eissenberg writes No Invading Allies Act
Ken Melvin writes A Developed Taste
Bill Haskell writes The North American Automobile Industry Waits for Trump and the Gov. to Act
A Chance to Modernize Health Care behind Bars, Section 1115 Medicaid Inmate Exclusion Waivers | NEJM, Brendan Saloner, Ph.D.
California and Washington are the first states to receive waivers from the Centers for Medicare and Medicaid Services (CMS) regarding the Medicaid Inmate Exclusion Policy. The policy generally prohibits Medicaid from paying for health care for people who are incarcerated. That being said, ~2 million Americans were incarcerated on any given day in 2020 and 2021.1 Disproportionately, people who are incarcerated are poor and members of a marginalized racial or of ethnic groups. They typically have elevated rates of mental illness, substance use disorders, and other chronic diseases.1 Engaging members of this population in better-coordinated care as they leave jail or prison could improve post release use of preventive and chronic-disease care at safety-net clinics and support improved health outcomes.
AB: The author is correct on the economic status of minorities. At the same time, there are no prisoners afforded the advantages of healthcare as would be found outside of prison. Even if they could, those who come from a better economic status must take what is offered to them. States must have healthcare for the incarcerated regardless of status. Medicaid would alleviate much of the state’s costs.
Under Section 1115 of the Social Security Act, CMS can grant states flexibility in statutory provisions on a demonstration basis. Section 1115 waivers of the Medicaid Inmate Exclusion Policy could demonstrate the viability of expanding Medicaid eligibility to people who are incarcerated presenting an important opportunity to modernize carceral health care in the United States. For example, the California waiver covers various reentry-related health services for an estimated 200,000 people per year during the 90 days before release from jail or prison.2 At least 13 additional states are seeking Inmate Exclusion waivers.2
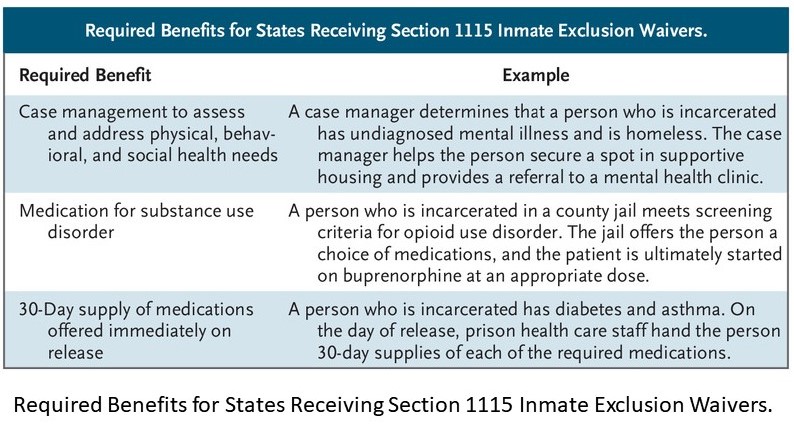
Providing coverage in a new context is a complicated undertaking for states. To support applications for such waivers, CMS released guidance in April 2023 outlining broad programmatic goals, including increased continuity of coverage and services, improved care coordination, and reduced hospital use and mortality in the post release period. The guidance lays out three required benefits:
- comprehensive case management,
- prerelease provision of medication for substance use disorder (CMS defined as medication-assisted treatment [MAT]) and,
- provision of a 30-day supply of all prescribed medications to people at the time of release (table).1 It also defines operational expectations related to data sharing, monitoring, and evaluation.
Beyond these required benefits, the CMS guidance is not especially prescriptive. For which, the lack of specificity may reflect the challenges associated with reforming carceral health care. In a prison environment, healthcare often operates with insufficient or sporadic staffing, tight budgets, and a limited set of covered services. Records for incarceration may not include the circumstances for incarceration.
For example, the length of confinement is often unpredictable. Early release is one example. States are working with CMS to define when people enter the period in which they would be eligible for Medicaid coverage pre-release. The guidance acknowledges many facilities will require a phase-in period to adapt to standard billing and reimbursement procedures.
There is also the reality of medical staffing in jails and prisons often does not meet community standards. CMS provides considerable flexibility in the required elements of the waivers. One such is the requirement to provide medication for substance use disorder. CMS urges programs “to use all available levers in their states to increase the availability of MAT as clinically appropriate.” One example covers the mandating of methadone and buprenorphine for all people who are incarcerated (as is required for Medicaid beneficiaries outside of carceral settings). These accommodations may be both necessary and beneficial in the short term, but it will be important for policymakers to recognize that federal funding provides critical leverage to improve the quality of carceral health care and to increase accountability among carceral agencies.
Ensuring that carceral health care is independently financed and operated would be one step toward modernizing care delivery. Health care contracts and budgets are generally overseen by security officials, many of whom have limited expertise in and experience with health care provision.
Security officials outsource care delivery to for-profit vendors competing for contracts by underbidding their competitors and ultimately skimp on services. Medicaid funding has the potential to disrupt this model. As a condition of receiving funds, carceral agencies could be required to establish a financially independent oversight board or management group that administers the health services benefit and makes decisions about covered benefits and staffing.
These requirements could be enforced by means of “conditions of participation” requirements that include governance standards similar to those applied to hospitals and other institutions that receive federal funding, which could help decouple the budgeting and operations of carceral health care from security operations.
In other high-income countries, carceral health care budgets are often administered by health agencies instead of corrections departments. For example, quality of care for people who were incarcerated improved when England shifted health care management from a prison authority to the National Health Service.3 It will always be necessary for carceral health care practitioners to collaborate with security staff. The establishing of operational independence could empower health care leaders to make coverage decisions without the need to accommodate or placate security officials and could support a clear division of responsibilities.
A second, related step would be to require ongoing, transparent health surveillance and quality-measurement programs as a condition of Medicaid funding. People who are incarcerated are currently excluded from all major national population-based health and health care surveys and statistics.4 States receiving Inmate Exclusion waivers will be required to compile data on Medicaid-funded services rendered under the waiver but aren’t slated to engage in broader, systematic data collection.
A bolder approach would be to require states and localities to compile health care claims data sets that meet reporting standards used by CMS programs outside of carceral facilities. The creation of such data sets could permit the development of claims-based quality-of-care measures that are relevant to people who are incarcerated. Such measures could be similar to those focused on preventive care and management of chronic diseases that are already widely used in the Healthcare Effectiveness Data and Information Set. This information would provide greater clarity about the ongoing health needs of people who are incarcerated and permit the establishment of benchmarks for assessing quality-improvement efforts.
Finally, over the long term, clinicians working in jails and prisons could be included in value-based payment programs that are now widespread in Medicaid. In recent years, there has been a proliferation of new Medicaid initiatives that provide supplements or alternatives to traditional fee-for-service volume-driven payment models. For example, Medicaid programs have implemented value-based initiatives in which a percentage of the total payment directed to providers or managed care organizations is conditioned on the attainment of particular quality metrics.5
Since incarceration often begins with a psychiatric or addiction-related crisis, value-based payments in jails and prisons could focus on crisis stabilization. Such efforts could reduce avoidable hospitalizations and improve continuity of medication use after release. Designing payment programs focused on improved post release outcomes is in keeping with the value proposition inherent in Inmate Exclusion waivers — that Medicaid can save some money during the reentry period by investing in better health care during incarceration. This goal may take time to realize, however, and up-front spending on better care-management systems in the shorter term may be required to increase the carceral system’s readiness to move toward value-based payment.
AB: The problem with this approach? Fifty states and fifty different approaches. The federal government could step in and mandate what is to be covered since it is footing most if not all of the costs.
The recent Inmate Exclusion waivers granted to California and Washington represent a meaningful step toward greater care integration for people who are incarcerated. Although, the California and Washington waivers cover a limited prerelease period, they could be a stepping stone to the partial or complete repeal of the Medicaid Inmate Exclusion Policy. One proposal with bipartisan support is under serious consideration in Congress. The repeal of this policy would represent an unprecedented investment of federal funds in the health of people who are incarcerated.
To ensure the investments made under future waivers or congressional action have the greatest possible effect, Medicaid officials could use the leverage associated with federal funding to improve the conditions under which health care is delivered in jails and prisons. Doing so could support the health of millions of Americans and the communities to which most of them will return.
Some Background Footnotes:
- Tsai D. Opportunities to test transition-related strategies to support community reentry and improve care transitions for individuals who are incarcerated. Centers for Medicare and Medicaid Services, April 17, 2023 (https://www.medicaid.gov/federal-policy-guidance/downloads/smd23003.pdf.
- Haldar S, Guth M. Section 1115 waiver watch: how California will expand Medicaid pre-release services for incarcerated populations. Kaiser Family Foundation, February 7, 2023 (https://www.kff.org/policy-watch/section-1115-waiver-watch-how-california-will-expand-medicaid-pre-release-services-for-incarcerated-populations/.
- Hutchings R, Davies M. How prison health care in England works. Nuffield Trust, October 20, 2021 (https://www.nuffieldtrust.org.uk/resource/prison-health-care-in-england.
- Wang EA, Macmadu A, Rich JD. Examining the impact of criminal justice involvement on health through federally funded, national population-based surveys in the United States. Public Health Rep 2019;134:Suppl:22S-33S.
- Lipson DJ, Au M, Stringer R, Vogt R. Accelerating the adoption of value-based payment in Medicaid by linking delivery system reform to managed care payment. Centers for Medicare and Medicaid Services, December 2019 (https://www.medicaid.gov/medicaid/downloads/accel-adoption-vp-pay.pdf.