American Journal of Public Health: “The Myth Regarding the High Cost of End-of-Life Care” December 2015, Melissa D. Aldridge, PhD, MBA and Amy S. Kelley, MD, MSHS There has been a lot of talk and presentation on End of Life care and its high costs. “The Myth Regarding the High Cost of End of Life Care” reviews those costs and expands the topic beyond End of Life to all the population with chronic conditions and functional limitations. FIGURE 1Estimated overlap between the population with the highest health care costs and the population at the end of life (United States, 2011). Source. Total population and health care costs were obtained from 2011 Medical Expenditure Panel Survey data and adjusted to include the nursing home population. The distribution of
Topics:
run75441 considers the following as important: Healthcare, Hot Topics, politics, run75441
This could be interesting, too:
Robert Skidelsky writes Lord Skidelsky to ask His Majesty’s Government what is their policy with regard to the Ukraine war following the new policy of the government of the United States of America.
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Joel Eissenberg writes No Invading Allies Act
Ken Melvin writes A Developed Taste
American Journal of Public Health: “The Myth Regarding the High Cost of End-of-Life Care” December 2015, Melissa D. Aldridge, PhD, MBA and Amy S. Kelley, MD, MSHS
There has been a lot of talk and presentation on End of Life care and its high costs. “The Myth Regarding the High Cost of End of Life Care” reviews those costs and expands the topic beyond End of Life to all the population with chronic conditions and functional limitations.
FIGURE 1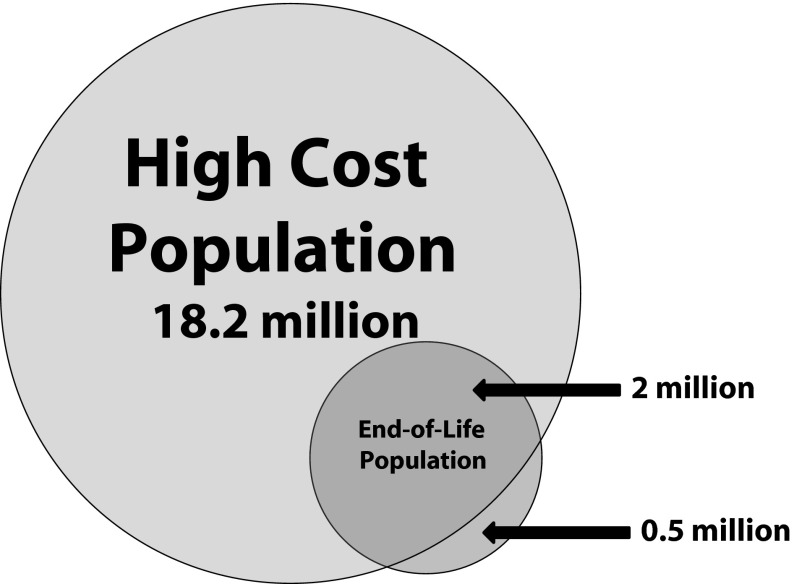 Estimated overlap between the population with the highest health care costs and the population at the end of life (United States, 2011). Source. Total population and health care costs were obtained from 2011 Medical Expenditure Panel Survey data and adjusted to include the nursing home population. The distribution of total costs for the end-of-life population was estimated from Health and Retirement Study data linked to Medicare claims data, adjusted to include non-Medicare payers, and adjusted to 2011 dollars utilizing BLS Consumer Price Index.
Estimated overlap between the population with the highest health care costs and the population at the end of life (United States, 2011). Source. Total population and health care costs were obtained from 2011 Medical Expenditure Panel Survey data and adjusted to include the nursing home population. The distribution of total costs for the end-of-life population was estimated from Health and Retirement Study data linked to Medicare claims data, adjusted to include non-Medicare payers, and adjusted to 2011 dollars utilizing BLS Consumer Price Index.
US population distribution of health care expenditures exhibits a significant “tail” segment of the population with extremely high costs. The study identifies 18.2 million individuals in the top 5% of total annual health care spending. These individuals incurred average annual health care expenditures of $17,500 or more per person and accounted for $976 billion in health care costs overall. Of these estimated 18.2 million individuals (5% of the population) who generate the highest annual costs, only 11% of the population (2 million individuals) are in the last year of life (Figure 1). Longitudinal analyses of spending reveal the population with the highest annual health care costs can be divided into 3 broad illness trajectories:
– Individuals who have high health care costs because it is their last year of life (population at the end of life),
– Individuals who experience a significant health event during a given year but who return to stable health (population with a discrete high-cost event), and
– Individuals who persistently generate high annual health care costs owing to chronic conditions, functional limitations, or other conditions. These individuals are not in the last year of life and live for several years generating high health care expenses (population with persistent high costs).
TABLE 1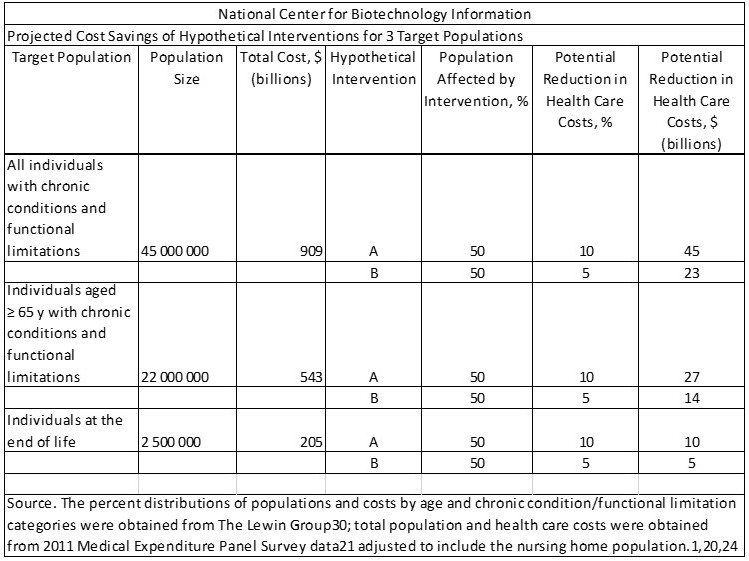 Melissa Aldridge and Amy Kelley: The identification of the appropriate target population for high-quality, cost-saving interventions is critical given the substantial variation in the size of different target populations, the costs generated by different populations, and the proportion of the target population likely to be affected by a specific intervention. Using data regarding the population with chronic conditions and functional limitations and our estimates with respect to the population at the end of life, we can imagine a hypothetical intervention and 3 potential target populations: individuals with chronic conditions and functional limitations, older adults with chronic conditions and functional limitations, and individuals at the end of life. If we assume, for instance, that the percentage of the target population that will be affected by the intervention is 50% and that the potential reduction in costs is 10%, we can compare between-intervention cost savings.
Melissa Aldridge and Amy Kelley: The identification of the appropriate target population for high-quality, cost-saving interventions is critical given the substantial variation in the size of different target populations, the costs generated by different populations, and the proportion of the target population likely to be affected by a specific intervention. Using data regarding the population with chronic conditions and functional limitations and our estimates with respect to the population at the end of life, we can imagine a hypothetical intervention and 3 potential target populations: individuals with chronic conditions and functional limitations, older adults with chronic conditions and functional limitations, and individuals at the end of life. If we assume, for instance, that the percentage of the target population that will be affected by the intervention is 50% and that the potential reduction in costs is 10%, we can compare between-intervention cost savings.
Putting to rest a meme; Many proposals to reduce health care costs in the United States target the high cost of end-of-life care. Yet at the population level, the cost of caring for individuals in their last year of life accounts for only 13% of total annual health care spending. Many believe or expect the majority of decedents in the highest cost group are in the last year of life; however, the majority of individuals in the group are not in their last year of life. Specifically, there is approximately 11% of the individuals in the highest cost group in the last year of life. Efforts to improve the quality of care for this group of 2 million are warranted; however, expecting such interventions to those in the last year of life to have a large impact on overall health care costs is misguided. Not only is this group small, but the window of time for a significant impact on costs is limited by the patients’ life expectancy.
If healthcare was to target those with chronic illness and functional limitations, the impact is 4 to 5 times greater than targeting those at end of life illness (Table 1).
Reference: American Journal of Public Health: “The Myth Regarding the High Cost of End-of-Life Care” December 2015, Melissa D. Aldridge, PhD, MBA and Amy S. Kelley, MD, MSHS
