I have been writing on healthcare for a while now and started to look at various topics with regard to pharmaceuticals. In my researching other topics, I found this particular correspondence to the Editor of the New England Journal of Medicine. Illuminating, if one might call it such? “A 1980 Letter on the Risk of Opioid Addiction” The NEJM published 1980 letter: Addiction Rare in Patients Treated with Narcotics Recently, we examined our current files to determine the incidence of narcotic addiction in 39,946 hospitalized medical patients who were monitored consecutively. Although there were 11,882 patients who received at least one narcotic preparation, there were only four cases of reasonably well documented addiction in patients who had no history of
Topics:
run75441 considers the following as important: Healthcare, Hot Topics, Journalism, run75441
This could be interesting, too:
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Joel Eissenberg writes No Invading Allies Act
Bill Haskell writes Families Struggle Paying for Child Care While Working
NewDealdemocrat writes January JOLTS report: monthly increases, but significant downward revisions to 2024
I have been writing on healthcare for a while now and started to look at various topics with regard to pharmaceuticals. In my researching other topics, I found this particular correspondence to the Editor of the New England Journal of Medicine. Illuminating, if one might call it such? “A 1980 Letter on the Risk of Opioid Addiction”
The NEJM published 1980 letter:
Addiction Rare in Patients Treated with Narcotics
Recently, we examined our current files to determine the incidence of narcotic addiction in 39,946 hospitalized medical patients who were monitored consecutively. Although there were 11,882 patients who received at least one narcotic preparation, there were only four cases of reasonably well documented addiction in patients who had no history of addiction. The addiction was considered major in only one instance. The drugs implicated were meperidine in two patients, Percodan in one, and hydromorphone in one. We conclude that despite widespread use of narcotic drugs in hospitals, the development of addiction is rare in medical patients with no history of addiction. Jane Porter; Herschel Jick; MD Boston Collaborative Drug Surveillance Program, Boston University Medical Center, Waltham, MA.
In a more recent June 1, 2017 letter to the NEJM editor, the authors dealt with the broad based and undocumented assumption in the 1980 letter of Addiction Rare in Patients Treated with Narcotics and the realization of the addiction and deaths of many people using Opioids. “from 1999 through 2015, more than 183,000 deaths from prescription opioids were reported in the United States and millions of Americans are now addicted to opioids.” Signed by four researchers exploring the reasons why Opioid addiction and deaths have risen, one of the conclusions reached was doctors being told “the risk of addiction was low when opioids were prescribed for chronic pain.” Supplementary Appendix.
From the 2017 correspondence to the Editor entitled; “A 1980 Letter on the Risk of Opioid Addiction,” the authors, by utilized bibliometric analysis of data derived from the number of citations of the 1980 letter from the date of its publication until March 30, 2017. The authors analyzed the relationship between the 1980 letter and it’s conclusion(s) with other document’s conclusions citing the 1980 letter. The analysis can be seen in Figure 1.
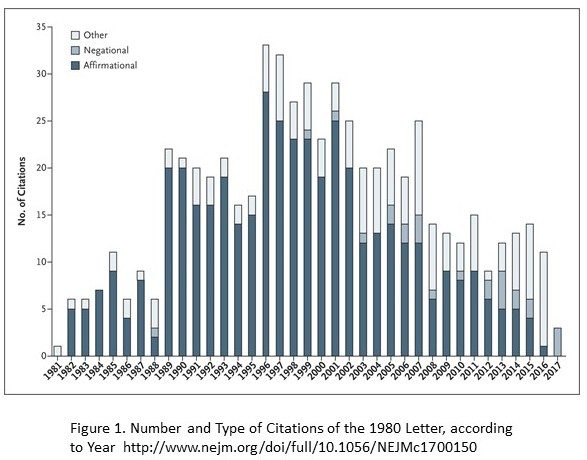 608 citations of the 1980 letter were identified (Figure 1) of the index publication. Also noted was a sizable increase in citations after the introduction of OxyContin (a long-acting formulation of oxycodone) in 1995. 439 (72.2%) authors of articles cited the 1980 letter as evidence addiction was rare in patients treated with opioids. 491 (80.8%) authors of articles did not note the patients described in the letter were hospitalized at the time they received the prescription and left readers to assume these were out-patients. As an aside to the citation of the letter, some authors grossly misrepresented the 1980 letter’s conclusion(s) in various comments as shown in Section 3, Supplementary Appendix. In comparison to the 1980 letter citations, the researchers also compared the number of times other letters published in the NEJM were cited: “11 other stand-alone letters taken from the same time period were cited at a median of 11 times.” To be redundant, the 1980 letter was cited 608 times.
608 citations of the 1980 letter were identified (Figure 1) of the index publication. Also noted was a sizable increase in citations after the introduction of OxyContin (a long-acting formulation of oxycodone) in 1995. 439 (72.2%) authors of articles cited the 1980 letter as evidence addiction was rare in patients treated with opioids. 491 (80.8%) authors of articles did not note the patients described in the letter were hospitalized at the time they received the prescription and left readers to assume these were out-patients. As an aside to the citation of the letter, some authors grossly misrepresented the 1980 letter’s conclusion(s) in various comments as shown in Section 3, Supplementary Appendix. In comparison to the 1980 letter citations, the researchers also compared the number of times other letters published in the NEJM were cited: “11 other stand-alone letters taken from the same time period were cited at a median of 11 times.” To be redundant, the 1980 letter was cited 608 times.
The researchers concluded:
“a five-sentence letter published in the Journal in 1980 was heavily and uncritically cited as evidence that ‘addiction was rare with long-term opioid therapy.’ Furthermore, they believed the citation pattern contributed to the North American opioid crisis by helping to shape a narrative lessening prescribers’ concerns about the risk of addiction associated with long-term opioid therapy. In 2007, the manufacturer of OxyContin and three senior executives pleaded guilty to federal criminal charges they had misled regulators, doctors, and patients about the risk of addiction associated with the drug. Our findings highlight the potential consequences of inaccurate citation and underscores the need for diligence when citing previously published studies.”
As I have been doing my research on another piece to which this is almost a prelude to it, I have found an overwhelming resistance to any type of control being placed on prescriptions for Opioids of which there are limitations on the number of days a prescription is given for short term pain. The naysayers always go back to the issue of chronic pain.
Whereas one perspective written in the NEJM Reducing the Risks of Relief — The CDC Opioid-Prescribing Guidline comes right out and states; “The few randomized trials to evaluate opioid efficacy for longer than 6 weeks had consistently poor results. In fact, several studies have showed that use of opioids for chronic pain may actually worsen pain and functioning, possibly by potentiating pain perception. A 3-year prospective observational study of more than 69,000 postmenopausal women with recurrent pain conditions showed that patients who had received opioid therapy were less likely to have improvement in pain (odds ratio, 0.42; 95% confidence interval [CI], 0.36 to 0.49) and had worsened function (odds ratio, 1.25; 95% CI, 1.04 to 1.51).”
The resistance to quantity limitations of Opioid prescriptions for non-chronic pain can be felt strongly in both state and federal legislatures by pharmaceutical companies lobbying. In a ten-year period from 2006 to 2015 Pharmaceutical companies have spent $880 million in lobbying all 50 state legislatures and in making campaign contributions in an effort to prevent laws restricting Opioid prescription quantities. In the end, it is just a matter of profits disguised as concern for chronic patient pain care.
