Angry Bear has been writing about the Opioid epidemic and what has been influencing it for years. I was to write on it at one time and continued to do so. It would seem there should be more coming forth from companies who promoted its use. If we go back and read the Jink and Porter letter misused to promote the use and sale of an Opioid, one can see how its use grew. billion is not enough to resolve the damage done. How billion in opioid settlement funds will be spent depends on these people, Shots – Health News, NPR, Aneri Pattani from KFF Health News As more than billion makes its way to state and local governments to compensate for the opioid epidemic, people with high hopes for the money are already fighting over a little-known
Topics:
run75441 considers the following as important: Healthcare, Hot Topics, KFF Health News, law, opioids, politics
This could be interesting, too:
Robert Skidelsky writes Lord Skidelsky to ask His Majesty’s Government what is their policy with regard to the Ukraine war following the new policy of the government of the United States of America.
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Joel Eissenberg writes No Invading Allies Act
Ken Melvin writes A Developed Taste
Angry Bear has been writing about the Opioid epidemic and what has been influencing it for years. I was to write on it at one time and continued to do so. It would seem there should be more coming forth from companies who promoted its use. If we go back and read the Jink and Porter letter misused to promote the use and sale of an Opioid, one can see how its use grew. $50 billion is not enough to resolve the damage done.
How $50 billion in opioid settlement funds will be spent depends on these people, Shots – Health News, NPR, Aneri Pattani from KFF Health News
As more than $50 billion makes its way to state and local governments to compensate for the opioid epidemic, people with high hopes for the money are already fighting over a little-known bureaucratic arm of the process: state councils that wield immense power over how the cash is spent.
In 14 states, these councils have the ultimate say on the money, which comes from companies that made, distributed, or sold opioid painkillers, including Purdue Pharma, Johnson & Johnson, and Walmart. In 24 other states, plus Washington, D.C., the councils establish budget priorities and make recommendations. Those will affect whether opioid settlement funds go, for example, to improve addiction treatment programs and recovery houses or for more narcotics detectives and prisons.
AB: Just to add a few more names to the list of companies promoting or distibuting Opioids; Miami-Luken, Amerisource Bergen Drug Co., Cardinal Health Inc. and McKesson Corp. The damage done in the past equates to over $1.5 trillion. They are walking away at $50 billion.
KFF Health News, along with Johns Hopkins University and Shatterproof, a national nonprofit focused on the addiction crisis, gathered and analyzed data on council members in all states to create the first database of its kind.
The data shows that councils are as unique as states are from one another. They vary in size, power, and the amount of funds they oversee. Members run the gamut from doctors, researchers, and county health directors to law enforcement officers, town managers, and business owners, as well as people in recovery and parents who’ve lost children to addiction.
“The overdose crisis is incredibly complex, and it demands more than just money,” said Rollie Martinson, a policy associate with the nonprofit Community Education Group, which is tracking settlement spending across Appalachia. “We also need the right people in charge of that money.”
That’s the $50 billion question: Are the right people steering the decisions? Already, criticism of the councils has been rife, with stakeholders pointing out shortcomings, from overrepresentation to underrepresentation and many issues in between. For example:
- Council membership doesn’t always align with the states’ hardest-hit populations — by race or geography.
- Heavy presence of specific professional groups — treatment providers, health care executives, or law enforcement officials, for example — might mean money gets directed to those particular interests at the expense of others.
- Few seats are reserved for people who’ve dealt with a substance use disorder themselves or supported a family member with one.
Find Out Who Is Controlling Opioid Settlement Cash in Your State
In 38 states and the District of Columbia, councils shape how opioid settlement dollars — totaling more than $50 billion nationwide — are spent. Council size and power vary by state.
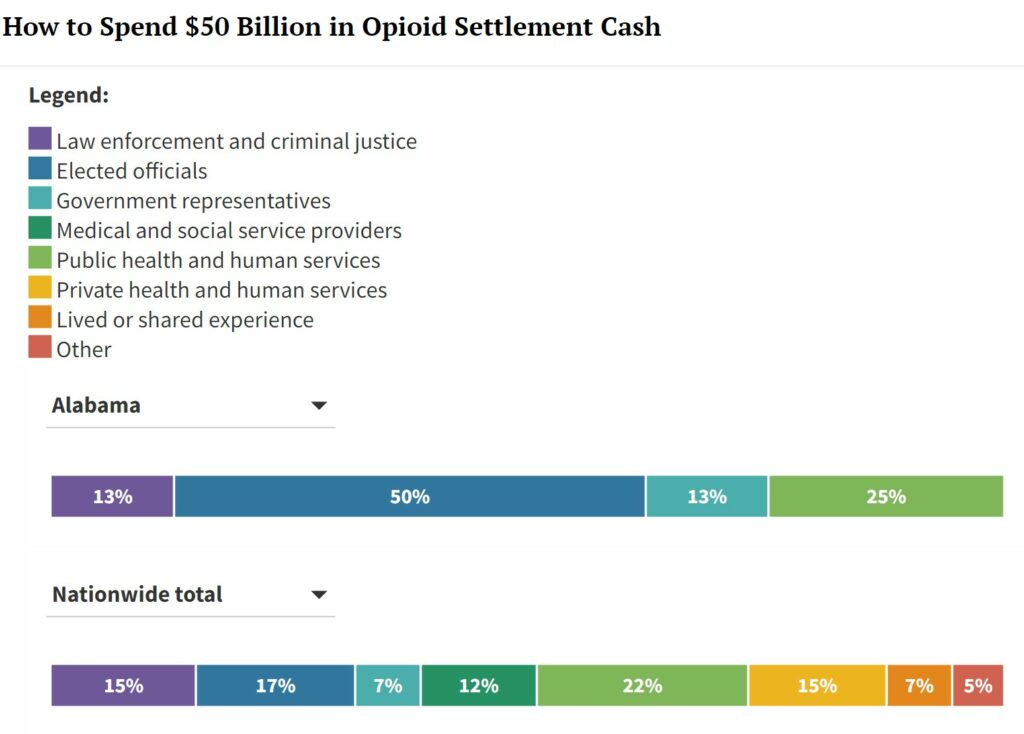
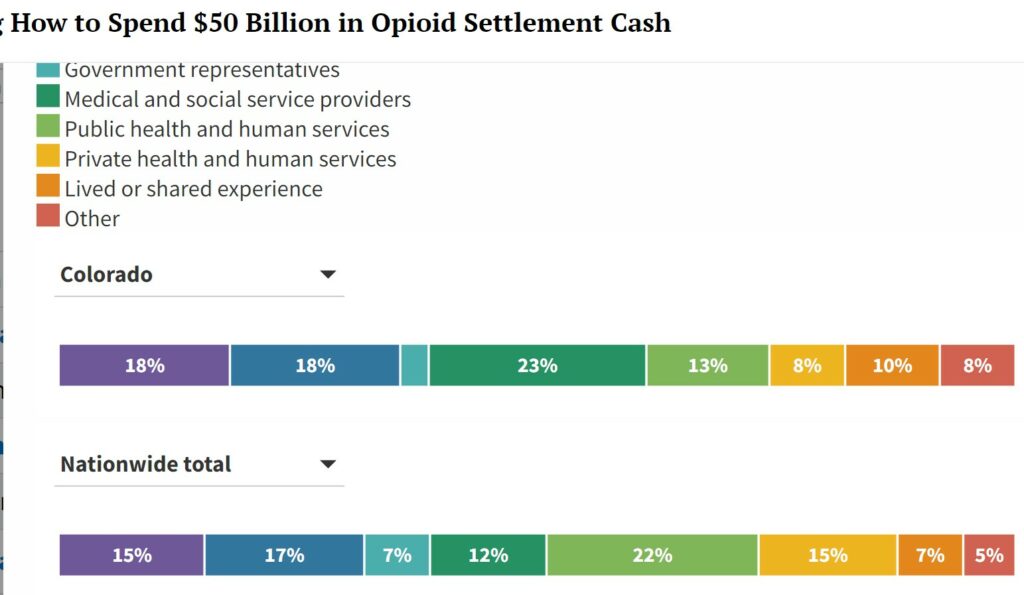
I was unable to recreate the flip chart showing all 38 states. I used the states of Alabama and Colorado to show how different states can establish their committees to handle their portion of the Opioid settlement funds. Having written on the topic for years now, the reality of the amounts comes to mind. The damage caused by these companies and which is still occurring is far more than $50 billion. As you can see, Alabama and Colorado have different methodologies to establish their committees. Alabama has 50% drawn from elected officials. Colorado has 18% from elected officials and 23% from Medical and Social Services. Alabama draws half of what Colorado does for Medical and Social Services. Where does each state place its priority? You can also match what each does against the nation’s overall ratios.
Across the country, council members generally fall into seven categories, but the ratios in which they’re represented differ greatly and offer clues about a state’s values. Percentages shown here are based on current membership rather than the category designations some states set for their councils.
Alabama:
Alabama: Council name: Oversight Commission on Alabama Opioid Settlement Funds Established by: Law
~~~~~~~~
Colorado
Across the country, council members generally fall into seven categories, but the ratios in which they’re represented differ greatly and offer clues about a state’s values. Percentages shown here are based on current membership rather than the category designations some states set for their councils.
Colorado has two councils. The Colorado Opioid Abatement Council, established by a memorandum of understanding, oversees 60% of the state’s settlement funds, which are controlled by regional boards, and has decision-making authority over an infrastructure fund that holds 10% of settlement funds. The Opioid Crisis Recovery Funds Advisory Committee, established by law, advises on 10% of settlement funds that are controlled by state government.
~~~~~~~~
The Charts (above) for each state can be found at the overall link to this KFF article. Credit for all the charts is to: KFF Health News’ Lydia Zuraw, Aneri Pattani, Colleen DeGuzman, and Megan Kalata; Shatterproof’s Kristen Pendergrass and Eesha Kulkarni; Johns Hopkins University’s Sara Whaley and Henry Larweh.
Admittedly, no one can design a perfect council. There’s no agreement on what that would even look like. But when a pile of money this big is at stake, everyone wants in on the action.
More than $3 billion of opioid settlement funds has already landed in government coffers, with installments to come through 2038. The money is meant as restitution for the hundreds of thousands of Americans who have died from drug overdoses in recent decades.
But what restitution looks like depends on whom you ask. People running syringe service programs might suggest spending money immediately on the overdose reversal medication naloxone, while hospital officials might advocate for longer-term investments to increase staffing and treatment beds.
“People naturally want money to go toward their own field or interest,” said Kristen Pendergrass, vice president of state policy at Shatterproof.
And that can trigger hand-wringing.
In many parts of the country, for instance, people who support syringe service programs or similar interventions worry that councils with high numbers of police officers and sheriffs will instead direct large portions of the money to buy squad cars and bulletproof vests. And vice versa.
In most states, though, law enforcement and criminal justice officials make up fewer than one-fifth of council members. In Alaska and Pennsylvania, for instance, they’re not represented at all.
Outliers exist, of course. Tennessee’s 15-member council has two sheriffs, one current and one former district attorney general, a criminal court judge, and a special agent from the state Bureau of Investigation. But like many other councils, it hasn’t awarded funds to specific groups yet, so it’s too soon to tell how the council makeup will influence those decisions.
Pendergrass and Johns Hopkins researcher Sara Whaley, who together compiled the list of council members, say criticism of councils drawing too heavily from one field, geographic area, or race is not just a matter of political correctness, but of practicality.
“Having diverse representation in the room is going to make sure there is a balance on how the funds are spent,” Pendergrass said.
To this end, Courtney Gary-Allen, organizing director for the Maine Recovery Advocacy Project, and her colleagues chose early on to ensure their state’s 15-member council included people who support what’s known as harm reduction, a politically controversial strategy that aims to minimize the risks of using drugs. Ultimately, this push led to the appointment of six candidates, including Gary-Allen, to the panel. Most have personal experience with addiction.
“I feel very strongly that if these six folks weren’t on the council, harm reduction wouldn’t get a single dollar,” she said.
Others are starting to focus on potential lost opportunities.
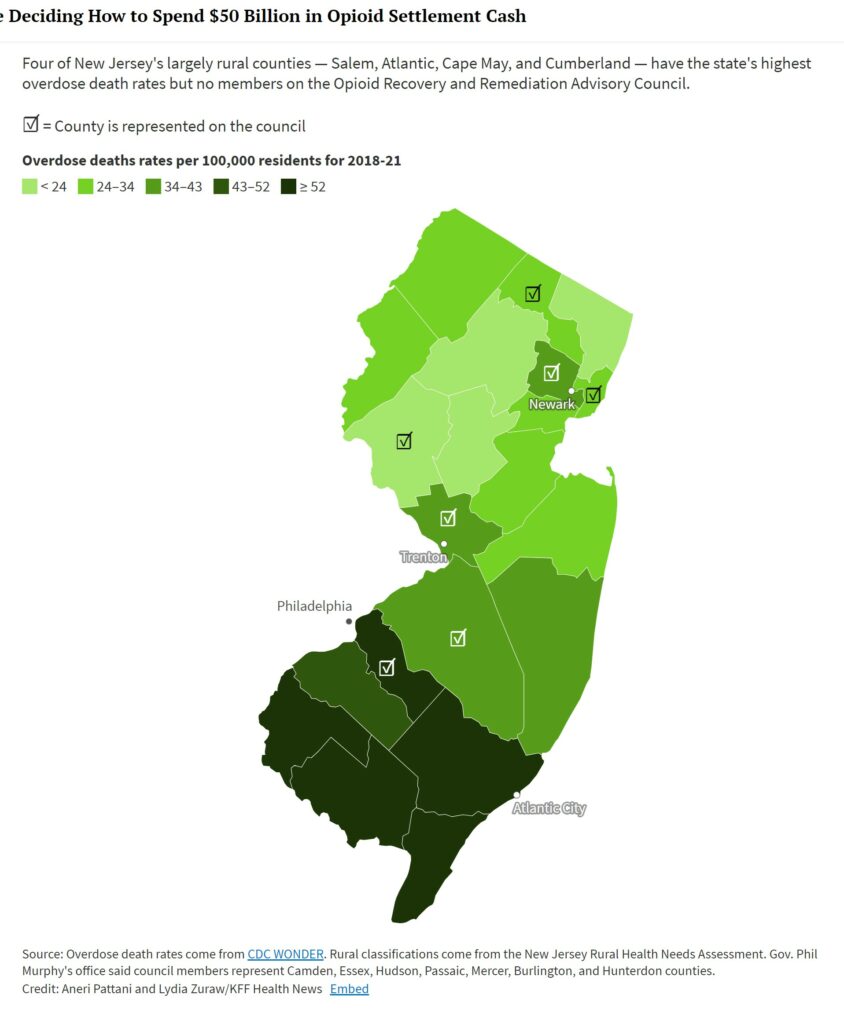
In New Jersey, Elizabeth Burke Beaty, who is in recovery from substance use disorder, has noticed that most members of her state’s council represent urban enclaves near New York City and Philadelphia. She worries they’ll direct money to their home bases and exclude rural counties, which have the highest rates of overdose deaths and unique barriers to recovery, such as a lack of doctors to treat addiction and transportation to faraway clinics.
Natalie Hamilton, a spokesperson for New Jersey Gov. Phil Murphy, a Democrat who appointed the members, said the council represents “a wide geographic region,” including seven of the state’s 21 counties.
But only two of those represented — Burlington and Hunterdon counties — are considered rural by the state’s Office of Rural Health needs assessment. The state’s hardest-hit rural counties lack a seat at the table.
Hard-Hit New Jersey Counties Lack Seats on Panel Overseeing Opioid Cash
Four of New Jersey’s largely rural counties — Salem, Atlantic, Cape May, and Cumberland — have the state’s highest overdose death rates but no members on the Opioid Recovery and Remediation Advisory Council.
☑ = County is represented on the council
Now that most of the council seats nationwide are filled, worries about racial equity are growing.
Louisiana, where nearly a third of the population is Black, has no Black council members. In Ohio, where Black residents are dying of overdoses at the highest rates, only one of the 29 council members is Black.
“There’s this perception that this money is not for people who look like me,” said Philip Rutherford, who is chief operating officer of Faces & Voices of Recovery and is Black. His group organizes people in recovery to advocate on addiction issues.
Research shows Black Americans have the fastest-rising overdose death rates and face the most barriers to gold-standard treatments.
In several states, residents have lamented the lack of council members with firsthand knowledge of addiction, who can direct settlement dollars based on personal experiences with the treatment and criminal justice systems. Instead, councils are saturated with treatment providers and health care organizations.
And this, too, raises eyebrows.
“Service providers are going to have a monetary interest,” said Tracie M. Gardner, who leads policy advocacy at the New York-based Legal Action Center. Although most are good people running good treatment programs, they have an inherent conflict with the goal of making people well and stable, she said.
“That is work to put treatment programs out of business,” Gardner said. “We must never forget the business model. It was there for HIV, it was there for covid, and it’s there for the overdose epidemic.”
Councils in South Carolina and New York have already seen some controversy in this vein — when organizations associated with members pursued or were awarded funding. It’s not a particularly surprising occurrence, since the members are chosen for their prominent work in the field.
Both states’ councils have robust conflict-of-interest policies, requiring members to disclose professional and financial connections. New York also has a law precluding council members from using their position for financial gain, and South Carolina uses a rubric to objectively score applications.
That these situations cause alarm regardless shows how much hope and desperation is tied up in this money — and the decisions over who controls it.
“This is the biggest infusion of funding into the addiction treatment field in at least 50 years,” said Gardner. “It’s money coming into a starved system.”