Brief recital of the costs and efforts of hospitals getting reimbursed by commercial healthcare insurance. It appears to be worsening. And the efforts to collect are costly. A Survey of Healthcare Insurance Practices Survey Methodology – 304 respondents, representing 772 hospitals, completed the survey. Not every respondent answered each question. All respondents are members of the American Hospital Association.– Web-survey administered between December 2021 and February 2022. Some participants opted to complete the survey using handwritten responses.– Results represent hospitals in 47 states. No responses were received from hospitals or health systems in New Mexico, Rhode Island, Vermont and Washington, D.C ~~~~~~~~ Payer
Topics:
Bill Haskell considers the following as important: Healthcare
This could be interesting, too:
Bill Haskell writes Families Struggle Paying for Child Care While Working
Joel Eissenberg writes RFK Jr. blames the victims
Joel Eissenberg writes The branding of Medicaid
Bill Haskell writes Why Healthcare Costs So Much . . .
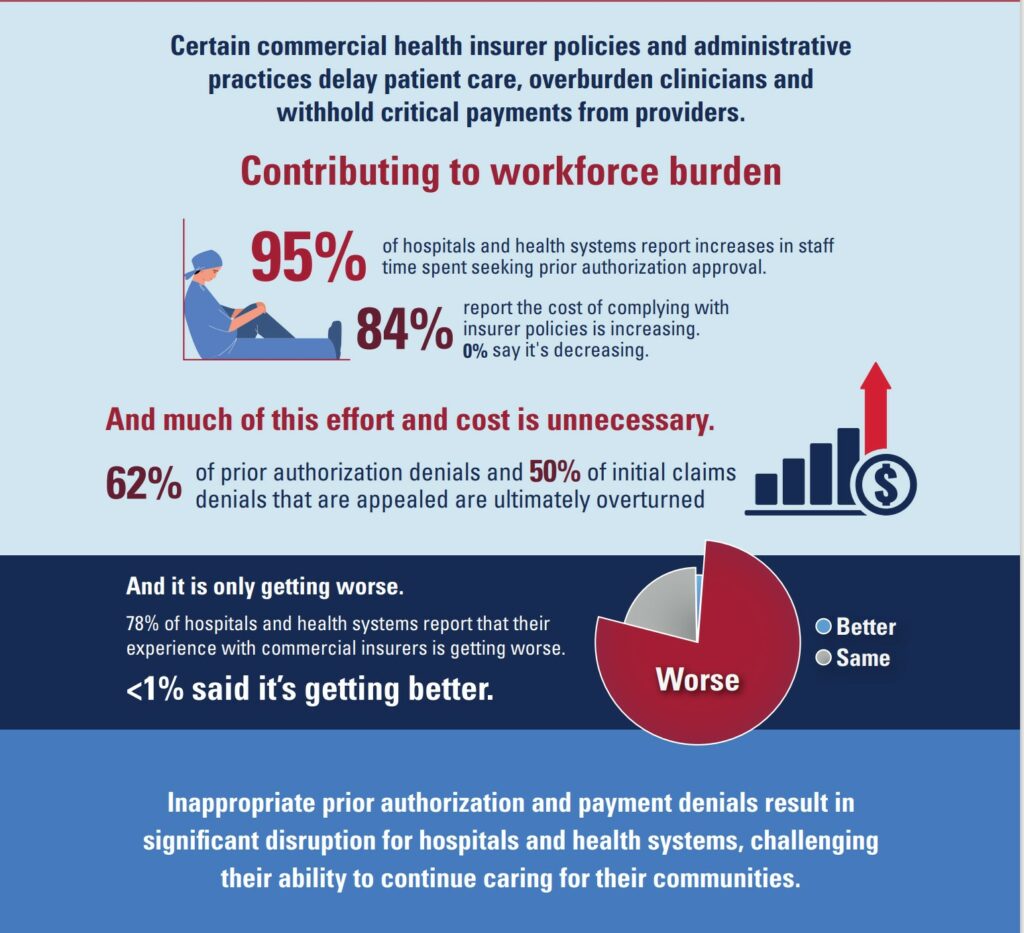
Brief recital of the costs and efforts of hospitals getting reimbursed by commercial healthcare insurance. It appears to be worsening. And the efforts to collect are costly.
A Survey of Healthcare Insurance Practices
Survey Methodology
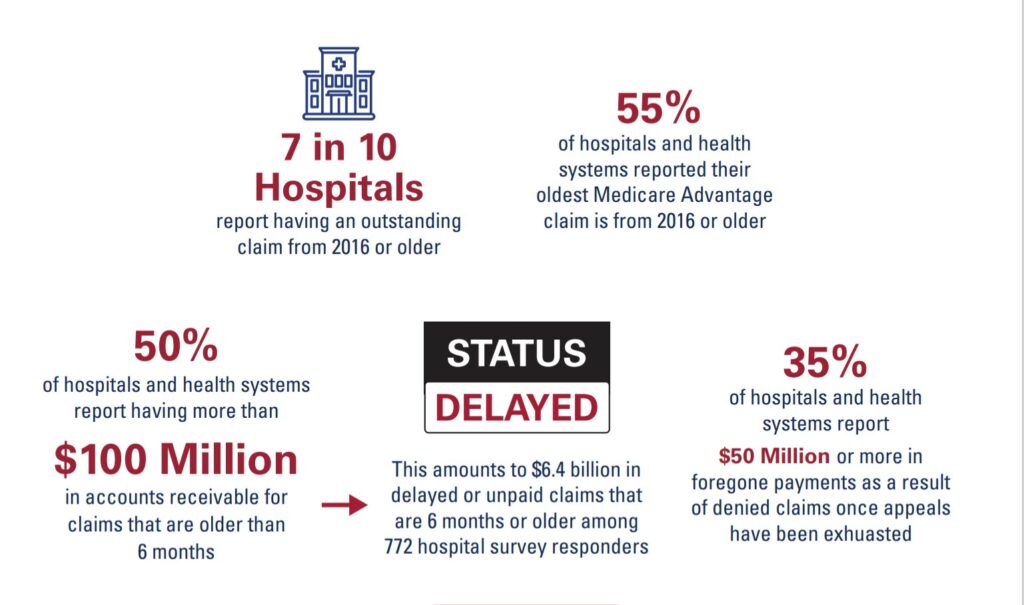
– 304 respondents, representing 772 hospitals, completed the survey. Not every respondent answered each question. All respondents are members of the American Hospital Association.
– Web-survey administered between December 2021 and February 2022. Some participants opted to complete the survey using handwritten responses.
– Results represent hospitals in 47 states. No responses were received from hospitals or health systems in New Mexico, Rhode Island, Vermont and Washington, D.C
~~~~~~~~
Payer denial tactics — how to confront a $20 billion problem
The high cost to health care providers to obtain reimbursement from insurers shows no signs of abating.
A recent report from the group purchasing and consulting organization Premier highlights the long-standing problem. It found that:
– Hospitals and health systems spent an estimated $19.7 billion in 2022 trying to overturn denied claims.
– Denied claims tended to be more prevalent for higher-cost treatments, with the average denial pegged to charges of $14,000 or more.
– Nearly 15% of all claims submitted to private payers initially are denied, including many that were preapproved during the prior authorization process. Overall, 15.7% of Medicare Advantage and 13.9% of commercial claims were initially denied.
– More than half of denied claims (54.3%) by payers ultimately were overturned but typically only after providers went through multiple rounds of costly appeals.
The high cost of reimbursement
The Premier findings track with the AHA’s most recent survey that was conducted between December 2021 and February 2022. In that survey, 78% of hospitals reported that their experience with commercial payers was getting worse.
Moreover, 84% of respondents said the cost of complying with insurer policies was increasing and 95% of hospitals and health systems reported that their staffs were spending more time on prior approval processes. Respondents also said that 62% of prior authorization denials and 50% of initial claims denials that were appealed were overturned.
The impact of some payer policies can cause dangerous delays in patient care, result in undue burden on providers and add billions of dollars in unnecessary cost to the nation’s health care system.
As health care organizations continue to face financial headwinds this year, the strategic imperative to manage claims denials effectively has become a higher priority in many organizations.