We are again discussing people on Medicaid who may not know they have to reenroll. The largest unknowing segment of that population are those over 65 years of age. This is a combination of several different articles on the Medicaid Disenrollment occurring today. Private business again taking advantage of the lack of knowledge of people and the situation. The Company Salivating Over The Medicaid Disaster (levernews.com), Matthew Cunningham-Cook Daniel Hatcher, a law professor at the University of Baltimore who has studied Maximus. “One of the big concerns is Maximus, a company really making money coming and going from county, state, and the federal governments. People benefiting the most are the company and occasionally governments, but not
Topics:
Bill Haskell considers the following as important: Education, Healthcare, Hot Topics, Medicaid Disaster, US EConomics
This could be interesting, too:
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Joel Eissenberg writes No Invading Allies Act
Bill Haskell writes The North American Automobile Industry Waits for Trump and the Gov. to Act
Bill Haskell writes Families Struggle Paying for Child Care While Working
We are again discussing people on Medicaid who may not know they have to reenroll. The largest unknowing segment of that population are those over 65 years of age. This is a combination of several different articles on the Medicaid Disenrollment occurring today. Private business again taking advantage of the lack of knowledge of people and the situation.
The Company Salivating Over The Medicaid Disaster (levernews.com), Matthew Cunningham-Cook
Daniel Hatcher, a law professor at the University of Baltimore who has studied Maximus.
“One of the big concerns is Maximus, a company really making money coming and going from county, state, and the federal governments. People benefiting the most are the company and occasionally governments, but not the people who are supposed to be benefiting from Medicaid services.”
Along with draining public finances, Maximus and other Medicaid redetermination contractors are incentivized to advocate for making Medicaid even more of a bureaucratic nightmare for recipients.
“If you look at the payment structure of these contracts, the more red tape made, the more money Maximus makes. The harder it is to get enrolled, the easier to get kicked off, and again the more money Maximus and contractors are making.”
Maximizing Profits
During the COVID-19 pandemic, lawmakers required states to stop removing people from Medicaid. Which every person knows is the national health insurance program for low-income Americans. The move led to record enrollment in a strictly means-tested program. A program designed to benefit only the very poor. Also a program from which people are often arbitrarily removed.
Late last year, Congress passed a bill of discontinuance and President Joe Biden signed a year-end spending bill directing states to resume annual redeterminations of Medicaid recipients’ eligibility for the program. Now, an estimated 17 million people, and potentially up to 24 million, face the prospect of losing coverage.
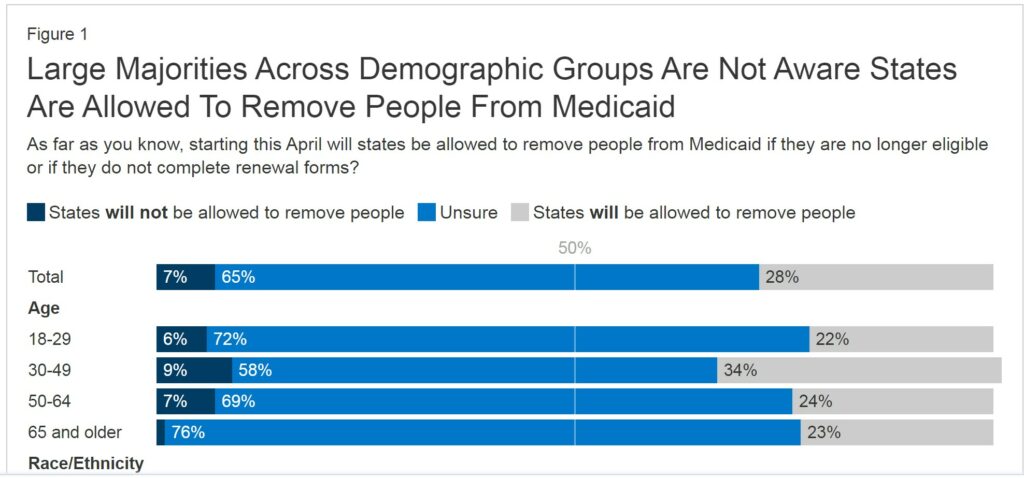
As I reported here, nearly half of Medicaid enrollees being disenrolled had not been through a Medicaid renewal process in the past. They were “that” new to the process. Included in this administrative snafu are the “two-thirds (68%) of Medicaid enrollees who are 65 and older and the more than half of Medicaid enrollees who are between the ages of 18 and 29 (53%).”
Source: KFF Survey of Health Insurance Consumers (Feb. 21-Mar. 14, 2023)
It has been determined, the expansion of Medicaid coverage reduces deaths, and also has a positive impact on people in poverty throughout their entire lives.
So as KFF determines the numbers of people not knowing they need to enroll again, the job for Maximus became far easier. Easy pickings if they do not reenroll.
While there are significant reporting gaps as to where Maximus is doing redeterminations and how states are reporting eligibility reviews, Maximus still dominates 60 percent of the Medicaid eligibility market, according to a recent report in Modern Healthcare.
While the final determinations for Medicaid eligibility must be completed by public employees, every other step of the process, from processing applications, to running call centers, to reaching out to people on the verge of losing benefits is done by private contractors.
In a recent investor presentation, Maximus wrote that it was boosting its “revenue and earnings guidance to account for Medicaid redeterminations,” and noted that “actual volume flow and beneficiary interaction will influence overall profitability.”
So far, more than 70 percent of those who have recently lost Medicaid coverage have been terminated for administrative reasons, such as not responding to a piece of mail or getting dropped from a call with a redetermination specialist, rather than because they were deemed ineligible due to their income and assets. Many of these people are likely still technically eligible for the program.
Maximus runs the call center for Medicaid eligibility in Indiana, where 85 percent of the 107,000 people kicked off Medicaid this year lost coverage because of procedural reasons. According to Maximus’ $400 million Indiana contract, up to seven percent of its eligibility calls in the state in a given week can be dropped before the company is penalized.
Maximus said in a statement to The Lever . . .
“We do not make Medicaid eligibility determinations. Our job is to support the states’ responsibilities to ensure that everyone who is eligible for Medicaid remains covered. If they are no longer eligible for Medicaid, we work with the states to refer them to other healthcare options such as the insurance marketplace. We are not paid in any state on the basis of whether an individual is found eligible or ineligible.”
Maximus did not answer follow-up questions about the scope of its work in various states and how much revenue the company expects to generate from its Medicaid redetermination business.
As Maximus seeks to expand its Medicaid redetermination work, the company has leaned into lobbying and political donations.
Maximus has donated $2.5 million to national political groups affiliated with state and local politicians since 2017. This includes $955,000 to the Republican Governors Association; $665,000 to the Democratic Governors Association; $450,000 to the Republican State Leadership Committee, which funnels money to GOP state legislative campaigns; $210,000 to the Republican Attorneys General Association; and $165,000 to the Democratic Attorneys General Association.
The company also donates to the National Governors Association, a nonpartisan group that represents governors from both parties.
Maximus spent $960,000 on federal lobbying alone in 2022, and its roster of lobbyists included former longtime Rep. Al Wynn (D-Md.). Wynn is now a senior director at the lobbying powerhouse Greenberg Traurig.
Wynn also was one of just a handful of members of the Congressional Black Caucus to vote “yes” on the final vote on the 1996 welfare reform bill. The legislation, which led to a doubling of extreme poverty, provided an enormous boon to Maximus by incentivizing the outsourcing of welfare eligibility work.
Shar Habibi, the research director of In The Public Interest, which advocates against privatization, said that Maximus’ role in Medicaid redeterminations will hollow out the government’s ability to effectively provide public services. She asked.
“When governments contract with firms like Maximus to do essential public functions like determining who is or isn’t eligible for Medicaid, the question gets raised:
Does outsourcing eligibility determination-related functions compromise the integrity of the program, especially when people’s lives are at stake? Using contractor staff does not promote an effective, efficient, and equitable delivery of Medicaid.”
Maximus also has major contracts with the federal government to provide assistance to those seeking to enroll in Medicare, the government health insurance program for seniors and those with disabilities, as well as those looking to sign up for individual health insurance plans offered on state marketplace exchanges created under Democrats’ 2010 health care law, the Affordable Care Act.
Some people formerly on Medicaid will move to exchange-based plans, which will almost certainly result in substantially higher out-of-pocket costs.
In May, Maximus laid off 700 workers from its Medicare and marketplace call centers where workers were seeking to unionize with the Communications Workers of America (CWA) union. The move led CWA to file an unfair labor practice charge with the National Labor Relations Board and launch a petition to pressure Secretary of Health and Human Services Xavier Becerra to investigate Maximus’ labor practices.
Meanwhile, Maximus’ government contracts to do such work have continued to expand under the Biden administration, despite the fact that Joe Biden pledged in his 2020 campaign that “I intend to be the most pro-union president leading the most pro-union administration in American history.” In September 2022, Maximus was awarded a $6.6 billion contract from the Center for Medicare and Medicaid Services (CMS) in September 2022.
Samira Burns, a spokesperson for the Health and Human Services Department (HHS), which includes CMS, told The Lever the department has initiated a request for information process with contractors like Maximus “to seek recommendations and remain in alignment with industry best practices to ensure we continue to meet national program missions and strategies. In recent years, there has been increasing labor concerns at certain call center locations. HHS/CMS is looking to explore ways to prevent or mitigate ongoing and future concerns.”