AB: This a good coverage on healthcare in the US as compared to other countries. It is long. It also has many charts and graphs rather than words. This is why I posted this at Angry Bear. It is easy to grasp the implications. U.S. Health Care from a Global Perspective, 2022, Commonwealth Fund, Munira Z. Gunja, Evan D. Gumas, Reginald D. Williams II Introduction In the previous edition of U.S. Health Care from a Global Perspective, we reported that people in the United States experience the worst health outcomes overall of any high-income nation.1 Americans are more likely to die younger, and from avoidable causes, than residents of peer countries. Between January 2020 and December 2021, life expectancy dropped in the U.S. and other
Topics:
Bill Haskell considers the following as important: Commonwealth Fund, Education, Global Perspective, Healthcare, Hot Topics, Part 2
This could be interesting, too:
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Joel Eissenberg writes No Invading Allies Act
Bill Haskell writes Families Struggle Paying for Child Care While Working
NewDealdemocrat writes January JOLTS report: monthly increases, but significant downward revisions to 2024
AB: This a good coverage on healthcare in the US as compared to other countries. It is long. It also has many charts and graphs rather than words. This is why I posted this at Angry Bear. It is easy to grasp the implications.
U.S. Health Care from a Global Perspective, 2022, Commonwealth Fund, Munira Z. Gunja, Evan D. Gumas, Reginald D. Williams II
Introduction
In the previous edition of U.S. Health Care from a Global Perspective, we reported that people in the United States experience the worst health outcomes overall of any high-income nation.1 Americans are more likely to die younger, and from avoidable causes, than residents of peer countries.
Between January 2020 and December 2021, life expectancy dropped in the U.S. and other countries.2 With the pandemic a continuing threat to global health and well-being, we have updated our 2019 cross-national comparison of health care systems to assess U.S. health spending, outcomes, status, and service use relative to Australia, Canada, France, Germany, Japan, the Netherlands, New Zealand, Norway, South Korea, Sweden, Switzerland, and the United Kingdom. We also compare U.S. health system performance to the OECD average for the 38 high-income countries for which data are available. The data for our analysis come from the Organisation for Economic Co-operation and Development (OECD) and other international sources (see “How We Conducted This Study” for details).
For every metric we examine, we used the latest data available. This means
that results for certain countries may reflect the height of the COVID-19 pandemic, when mental health conditions were surging, essential health services were disrupted, and patients may not have received the same level of care.3
Highlights
- Health care spending, both per person and as a share of GDP, continues to be far higher in the United States than in other high-income countries. The U.S. is the only country not having universal healthcare..
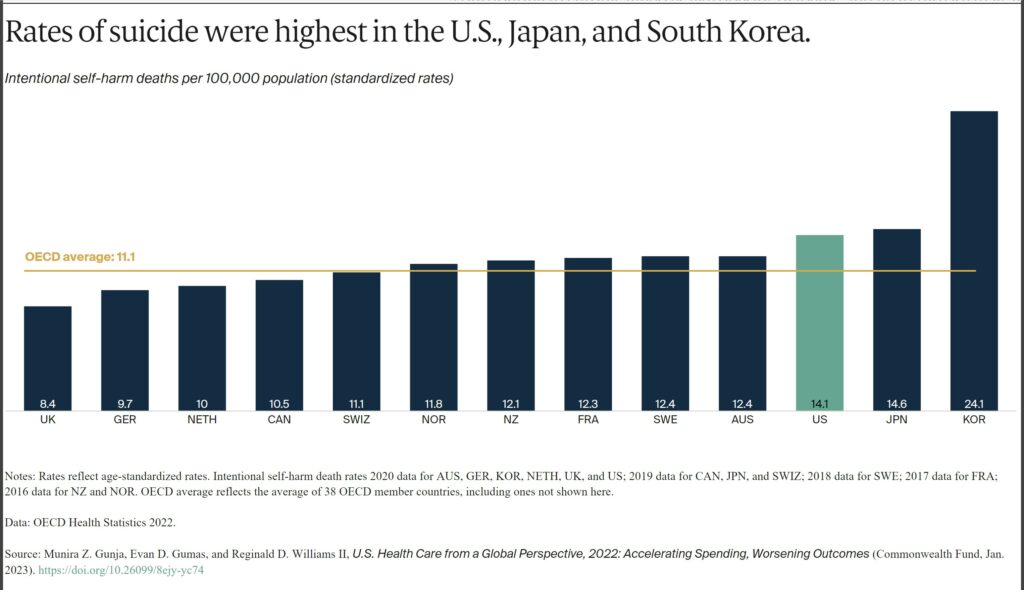
- The U.S. has the lowest life expectancy at birth, the highest death rates for avoidable or treatable conditions, the highest maternal and infant mortality, and among the highest suicide rates.
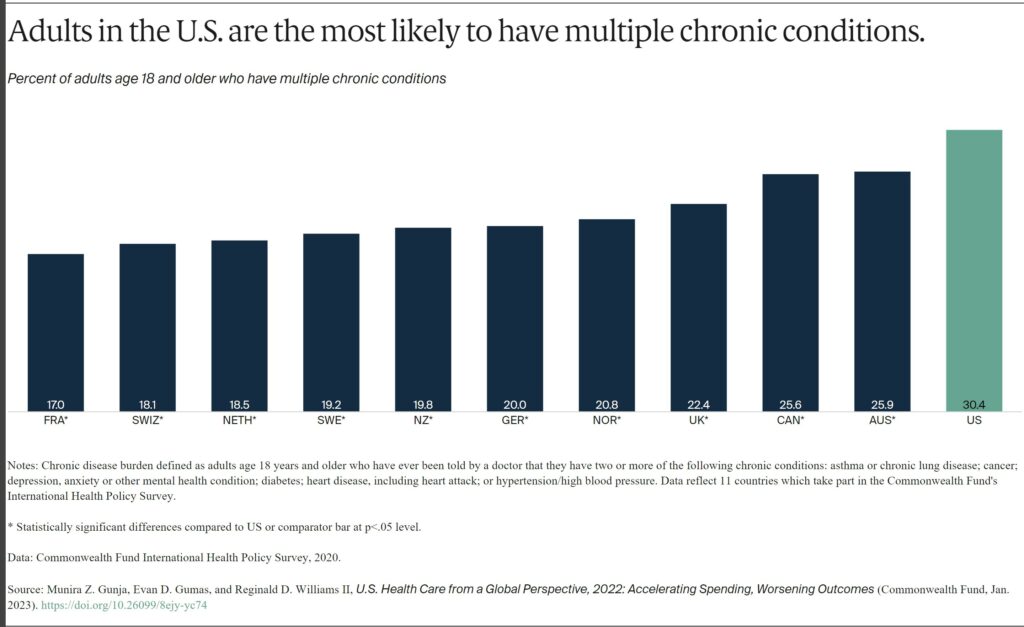
- The U.S. has the highest rate of people with multiple chronic conditions and an obesity rate nearly twice the OECD average.
- Americans see physicians less often than people in most other countries and have among the lowest rate of practicing physicians and hospital beds per 1,000 population.
- Screening rates for breast and colorectal cancer and vaccination for flu in the U.S. are among the highest, but COVID-19 vaccination trails many nations.
Findings
Health Care Spending and Coverage
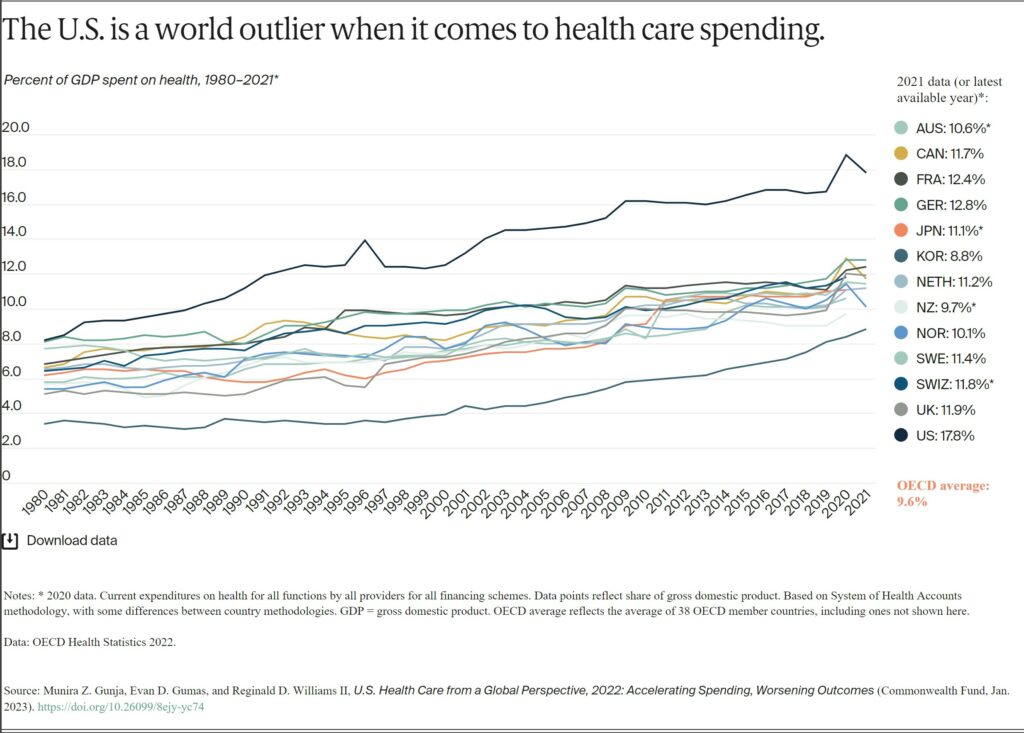
In all countries, health spending as a share of the overall economy has been steadily increasing since the 1980s, as spending growth has outpaced economic growth.4 This growth is in part because of medical technologies, rising prices in the health sector, and higher demand for services.5 In 2020, when the COVID-19 pandemic began, health care spending rose rapidly in nearly all countries. Governments sought to mitigate the spread of the disease through COVID testing, vaccine development, relief funds, and other measures.6 Since then, spending has slowed but still remains higher from years prior.7
In 2021, the U.S. spent 17.8 percent of gross domestic product (GDP) on health care, nearly twice as much as the average OECD country.
AB: In spite of predictions and forecasts, spending has hovered around 17% with the exceptio of during the pandemic.
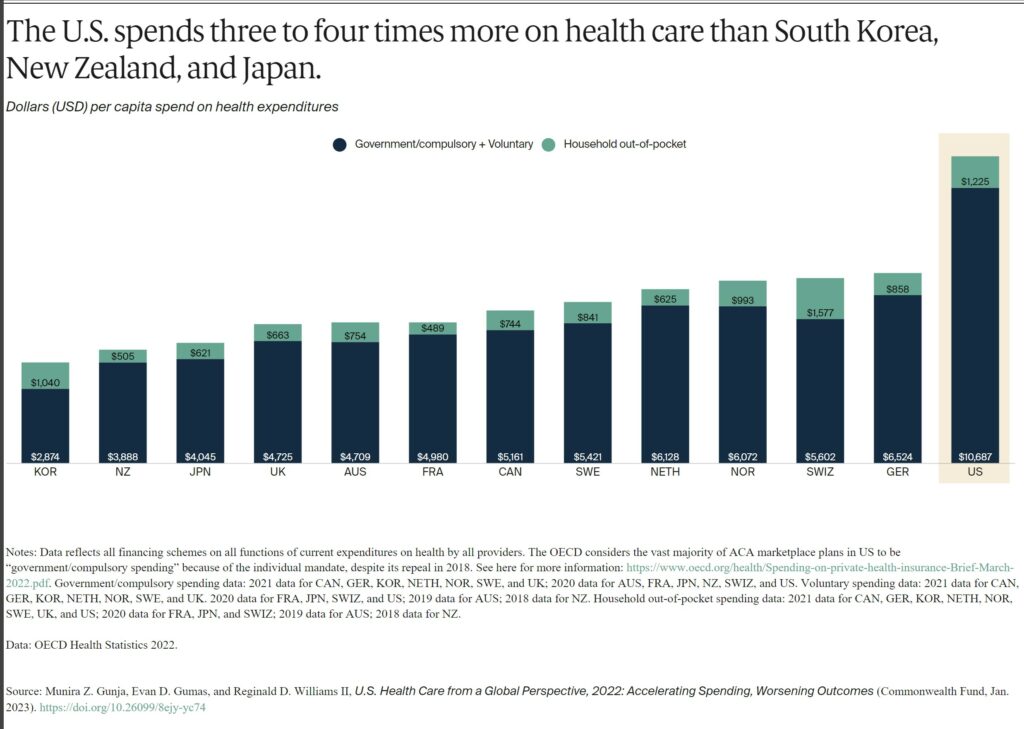
Health spending per person in the U.S. was nearly two times higher than in the closest country, Germany. It was also four times higher than in South Korea. This includes spending for people in public programs such as Medicaid, Children’s Health Insurance Program, Medicare, and military plans. It includes spending by those with private employer-sponsored coverage or other private insurance plus out-of-pocket health spending.
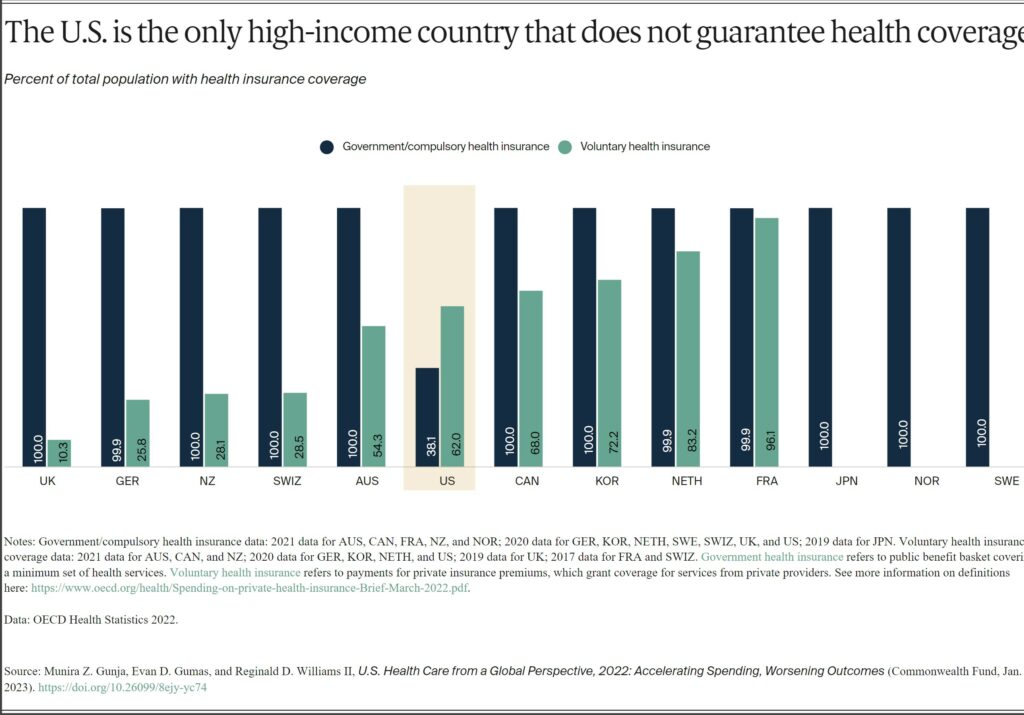
Except for the US, all the countries in this analysis guarantee government, or public, health coverage to all their residents. In addition to public coverage, people in several of the countries have the option to also purchase private coverage. In France, nearly the entire population has both private and public insurance.
In 2021, 8.6 percent of the U.S. population was uninsured.8 The U.S. is the only high-income country where a substantial portion of the population lacks any form of health insurance.
Health Outcomes
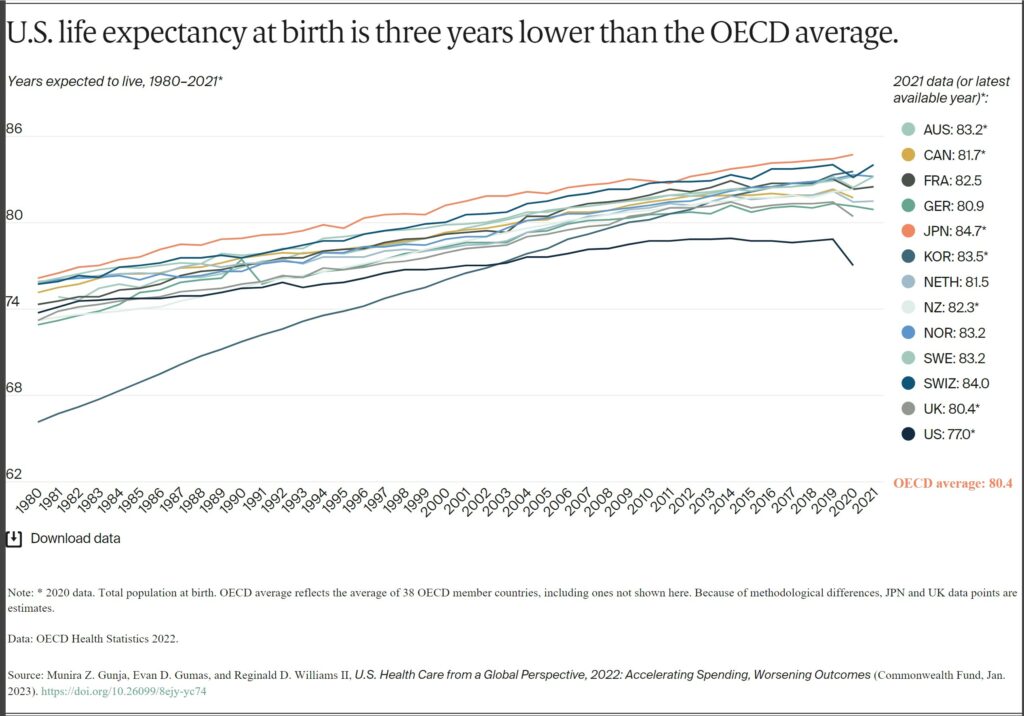
Despite high U.S. spending, Americans experience worse health outcomes than their peers around world. For example, life expectancy at birth in the U.S. was 77 years in 2020. This is three years lower than the OECD average. Provisional data shows life expectancy in the U.S. dropped even further in 2021.9
Life expectancy in the US masks racial and ethnic disparities.10 Average life expectancy in 2019 for non-Hispanic Black Americans (74.8 years) and non-Hispanic American Indians or Alaska Natives (71.8 years) is four and seven years lower, respectively, than it is for non-Hispanic whites (78.8 years).
Meanwhile, life expectancy for Hispanic Americans (81.9 years) is higher than it is for whites and similar to life expectancy in the Netherlands, New Zealand, and Canada. As a group, Asian Americans have a higher life expectancy (85.6 years) than people in Japan.
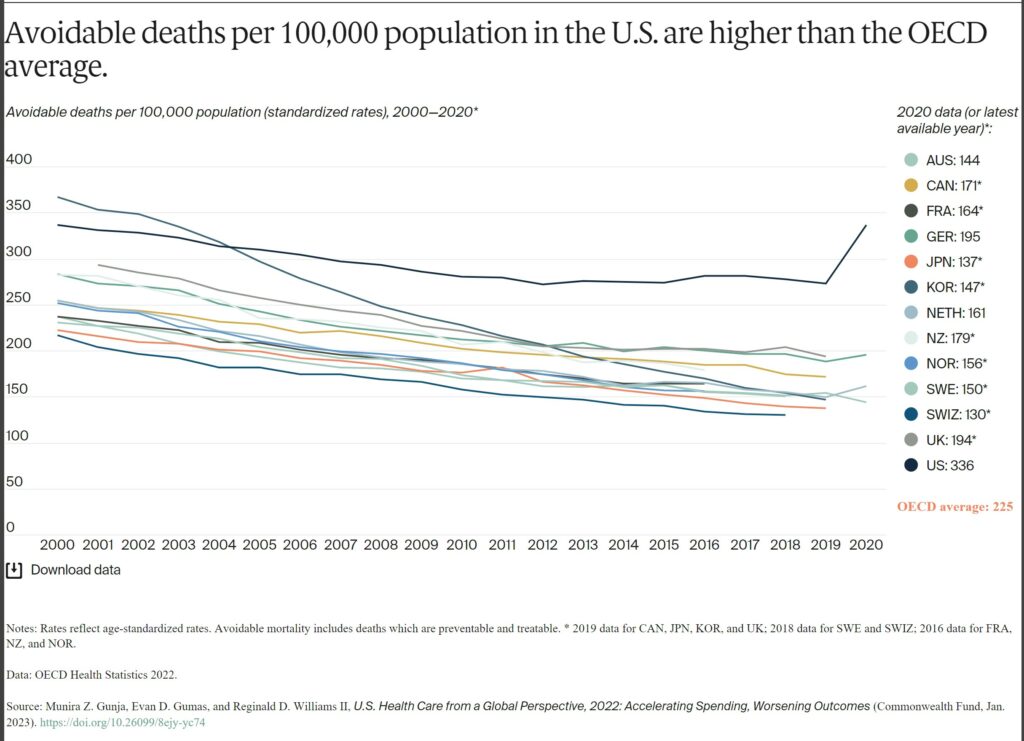
Avoidable mortality refers to preventable deaths and treatable illness. Preventable deaths can be avoided through effective public health measures and through primary prevention, such as nutritional diet and exercise. Treatable mortality can be avoided mainly through timely and effective health care interventions, including regular exams, screenings, and treatment.11 Since 2015, avoidable deaths have been on the rise in the U.S., which had the highest rate in 2020 of all the countries in our analysis.
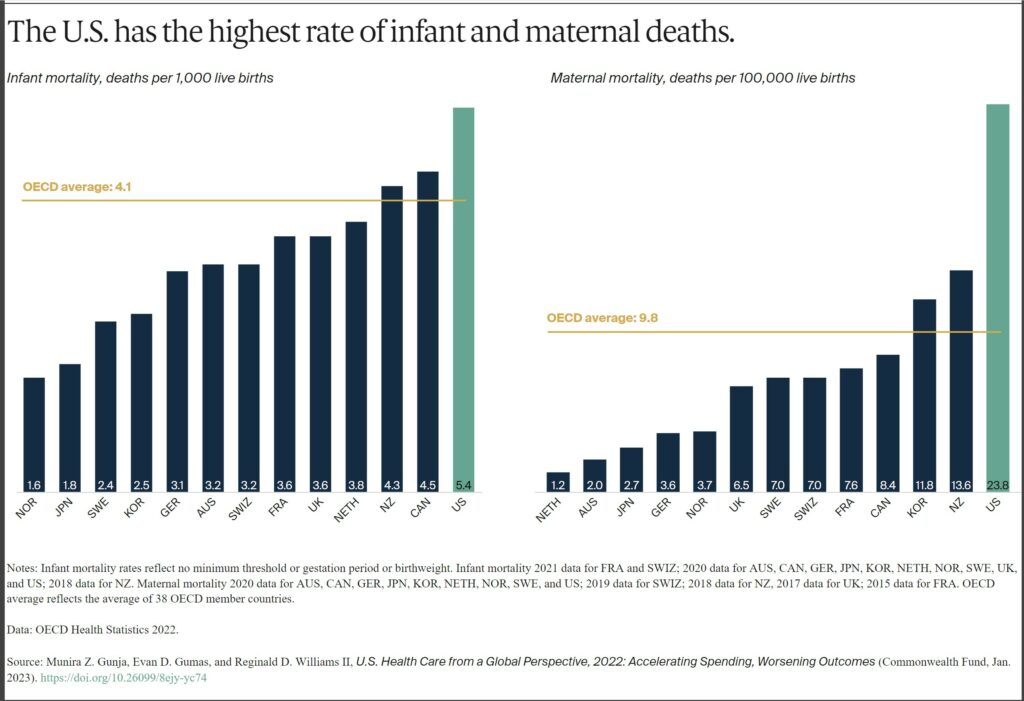
In 2020, the infant mortality rate in the U.S. was 5.4 deaths per 1,000 live births, the highest rate of all the countries in our analysis. In contrast, there were 1.6 deaths per 1,000 live births in Norway.
Women in the U.S. have experienced the highest rate of maternal mortality related to complications of pregnancy and childbirth. In 2020, there were nearly 24 maternal deaths for every 100,000 live births in the U.S., more than three times the rate in most other high-income countries we studied. A high rate of cesarean section, inadequate prenatal care, and socioeconomic inequalities contributing to chronic illnesses like obesity, diabetes, and heart disease may all help explain high U.S. infant and maternal mortality.12
AB: I will add to this. Biden’s maternal healthcare policy was extended to one year for Medicaid (unless some one tells me differently). As I wrote in “A Woman’s Right to Safe Healthcare Outcomes, Angry Bear” giving birth to a child is more dangerous in the US. I was fortunate to watch the birth of my three. This occurs even if you have a good healthcare policy.
Having dramatically increased during the COVID-19 pandemic, suicide rates can indicate a high burden of mental illness.13 The U.S. has the third-highest suicide rate, while the U.K. has the lowest — nearly half the U.S. rate.
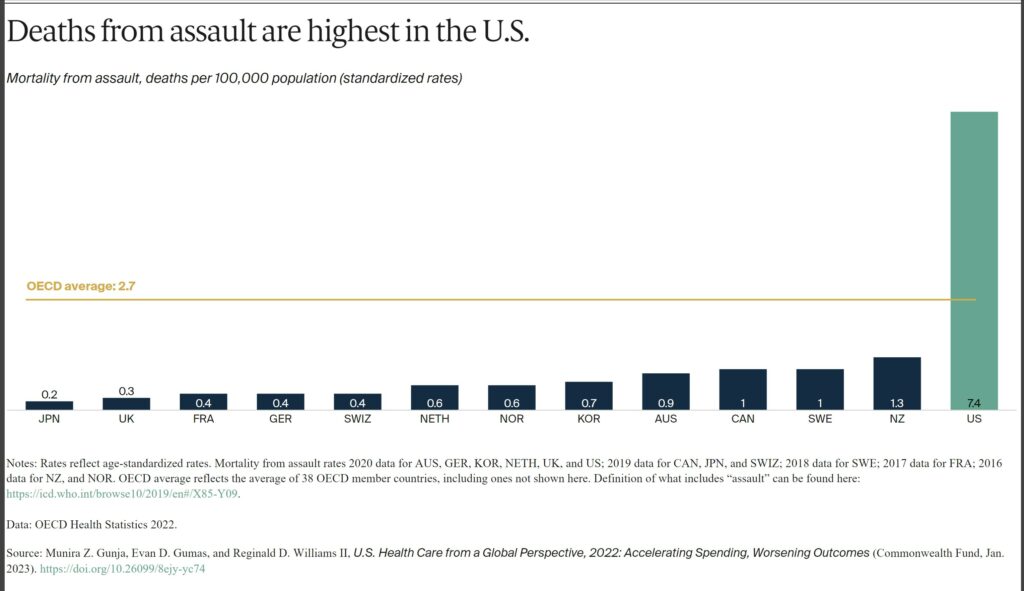
The U.S. is an outlier in deaths from physical assault, which includes gun violence. Its 7.4 deaths per 100,000 people is far above the OECD average of 2.7, and at least seven times higher than all other high-income countries in our study, except New Zealand.
Health Status
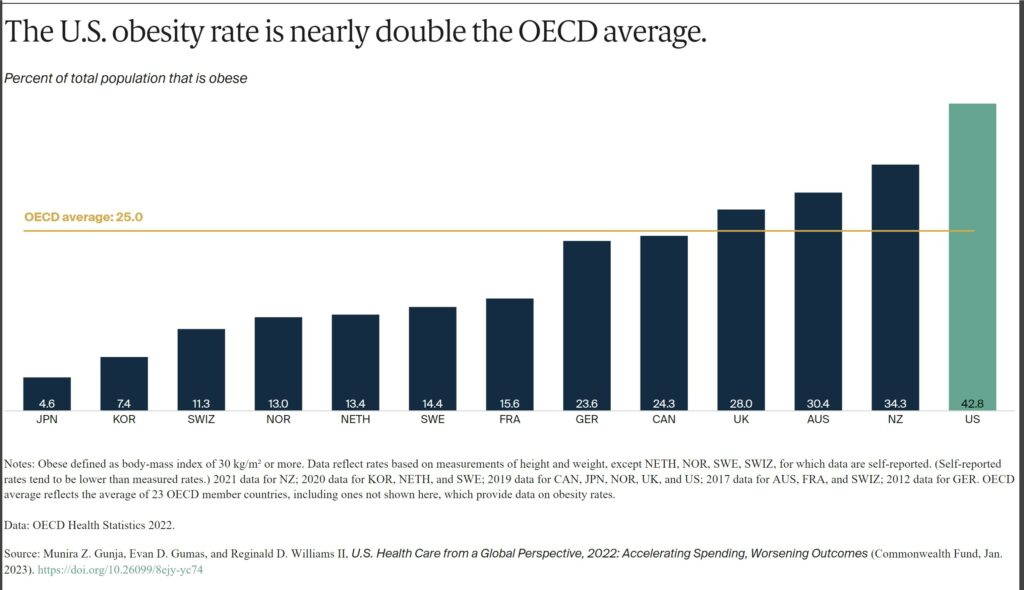
Obesity is a key risk factor for chronic conditions such as diabetes, hypertension and other cardiovascular diseases, and cancer. Issues contributing to obesity include unhealthy living environments, poor diet, food and agricultural sectors, lower socioeconomic status, and higher rates of behavioral health problems.14
The U.S. has the highest obesity rate among the countries we studied, where data was available — nearly two times higher than the OECD average.
In 2020, three of 10 U.S. adults surveyed said at some point in their lifetime they had been diagnosed with two or more chronic conditions such as asthma, cancer, depression, diabetes, heart disease, or hypertension. No more than a quarter of residents in the other countries studied reported the same, and the U.S. rate was nearly twice as high as France’s.
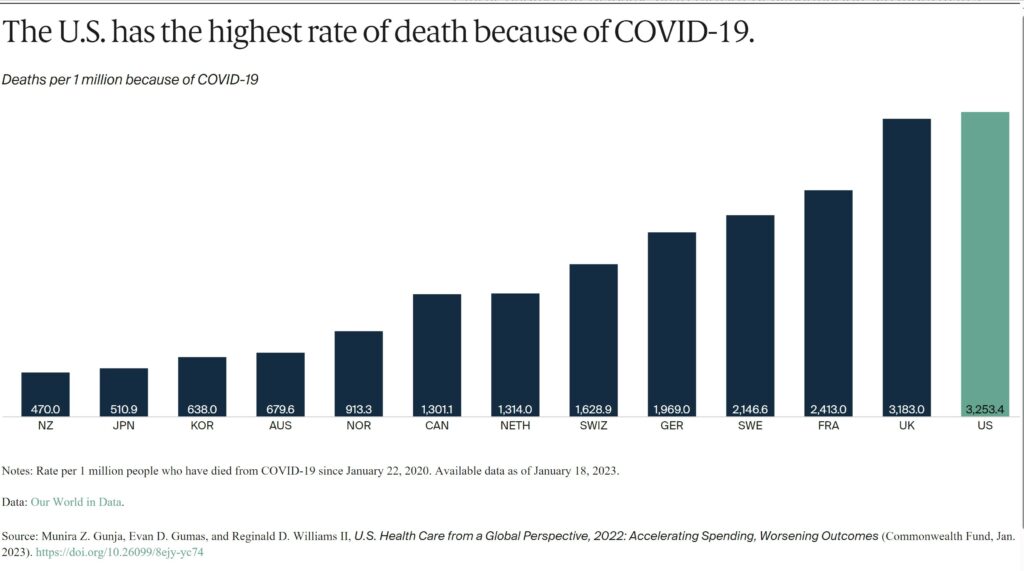
Since the start of the COVID-19 pandemic, more people in the U.S. have died from the coronavirus than in other high-income countries. For every 1 million cases between January 22, 2020, and January 18, 2023, there were more than 3,000 deaths in the U.S.
Health Care Use
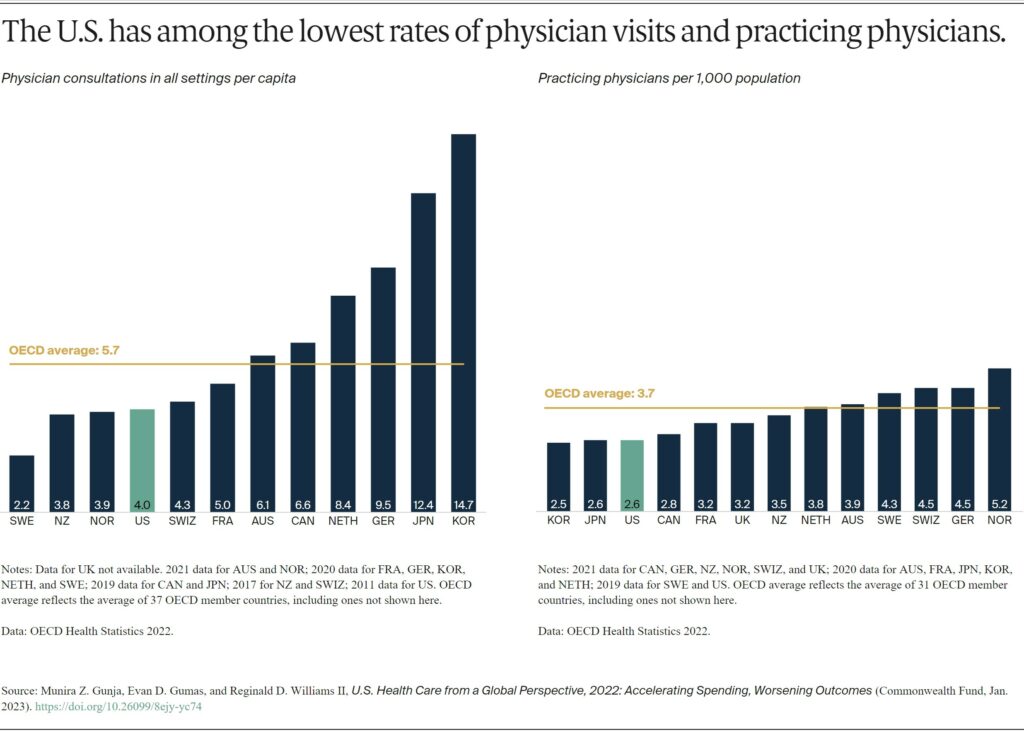
While U.S. health care spending is the highest in the world, Americans overall visit physicians less frequently than residents of most other high-income countries. At four visits per person per year, Americans see the doctor less often than the OECD average.
Less-frequent physician visits may be related to the comparatively low supply of physicians in the U.S., which is below the average number of practicing physicians in OECD countries.
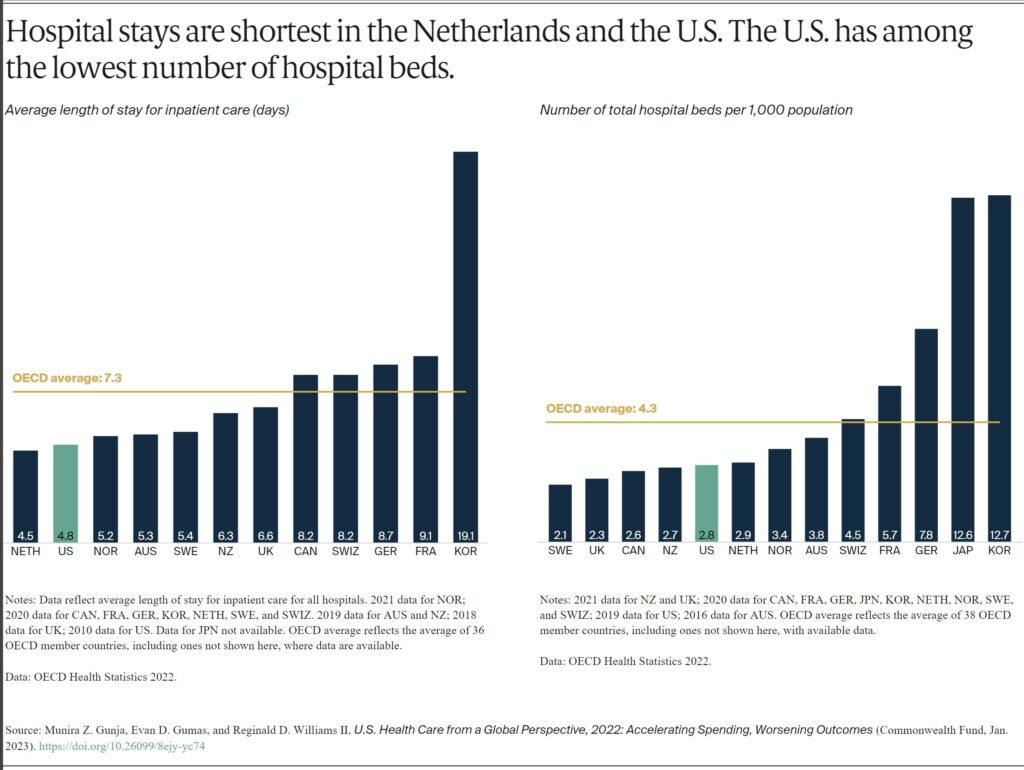
The average length of a hospital stay in the U.S. for all inpatient care was 4.8 days. This is far lower than the OECD average. The U.S. had 2.8 hospital beds per 1,000 population, lower than the OECD average of 4.3.
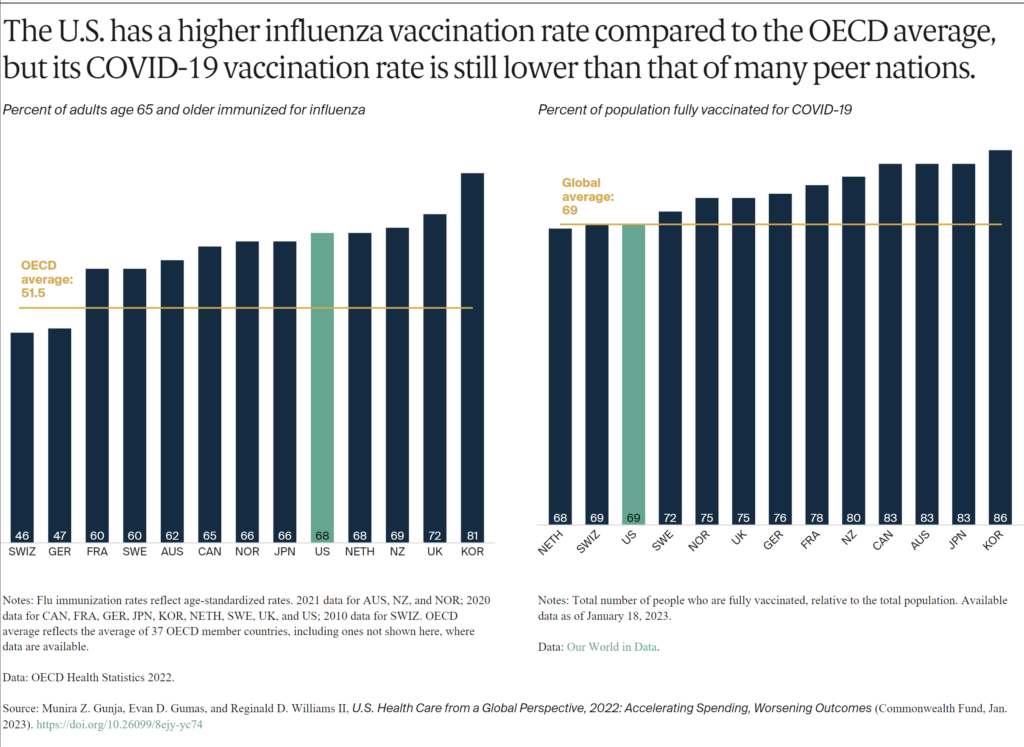
More than two-thirds of older Americans receive the flu vaccine. This is similar to older residents of several other high-income countries, and more than the OECD average.
The U.S., however, has one of the lowest COVID-19 vaccination rates among high-income countries. As of January 2023, 69 percent of the population were fully vaccinated, compared to 86 percent in South Korea, although rates are regularly being updated.
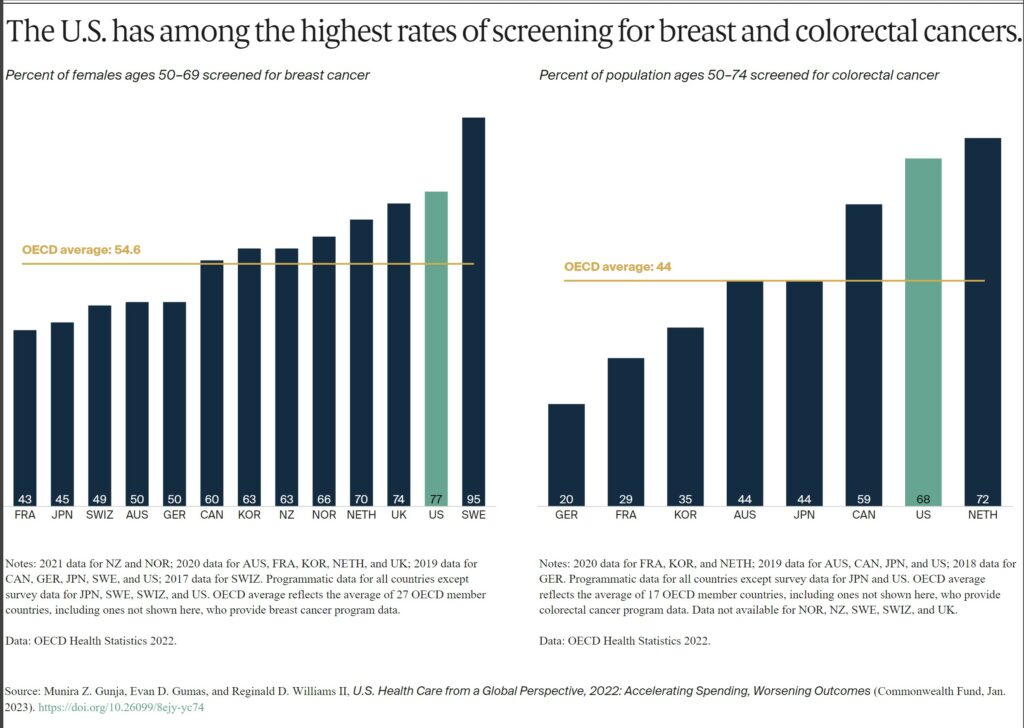
The U.S. does relatively well with cancer prevention. This is likely a reflection of extensive screening and detection. Such measures are a key to diagnosing breast and colorectal cancers early and beginning treatment in a timely manner.15
The U.S. and Sweden had the highest number of breast cancer screenings among women ages 50 to 69 and notably higher than the OECD average. In contrast, just 43 percent of women ages 50 to 69 were screened in France. When it comes to colorectal cancer screening, the U.S. exceeded the OECD average and had among the highest rates.
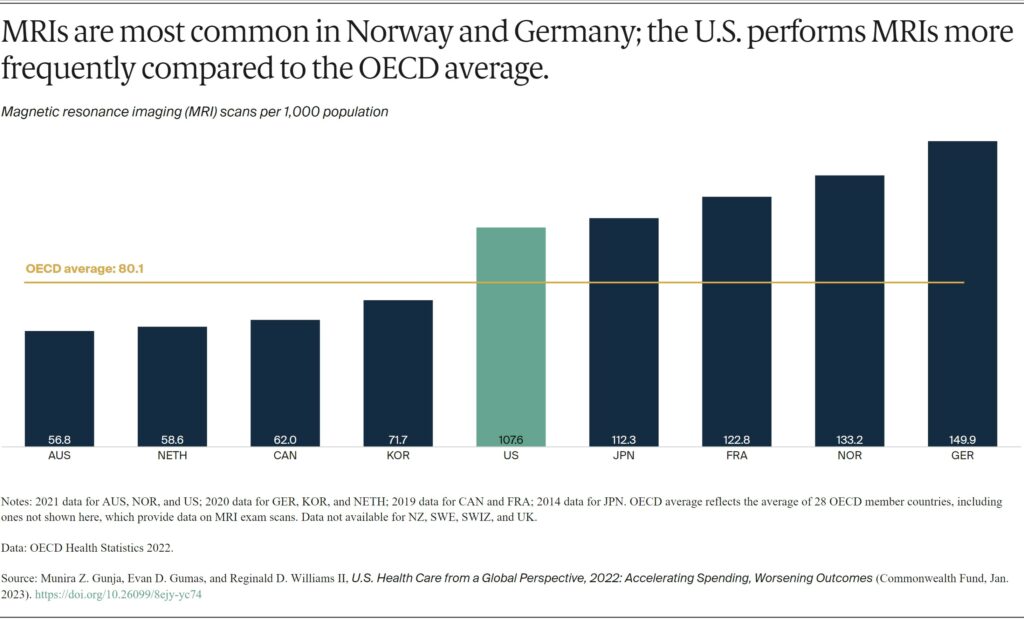
Magnetic resonance imaging (MRI) is a common and effective imaging technique for diagnosing and tracking the treatment of a variety of illnesses. The countries using these specialized scans the most are the U.S., Japan, France, Norway, and Germany, with more than 100 scans per 1,000 people.
The U.S. has a high number of MRI units available to physicians, about 38 units for every 1 million people in 2018. That’s the second-highest rate in the world behind Japan, which has 51.7 units per 1 million people.16
The clinical benefit as a diagnostic tool are well documented. MRIs are also particularly expensive in the U.S., averaging $1,119.17 The cost is 42 percent more than the U.K.’s average cost and 420 percent more than Australia’s. And while MRIs are accessible in the U.S., Americans spend far more on them than their international peers do.18
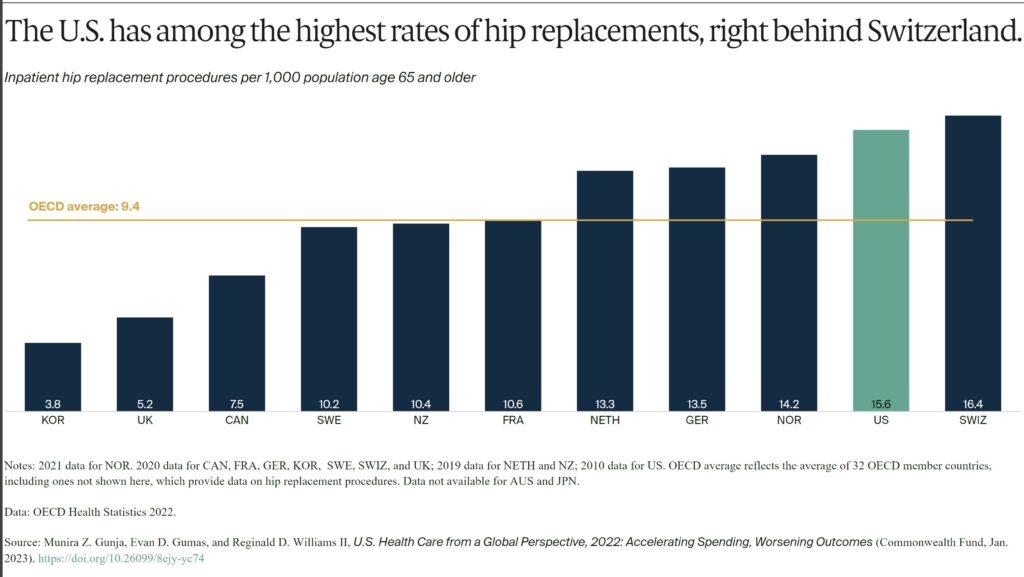
Globally, the rates of hip replacement are increasing as populations age and develop conditions such as osteoarthritis. It is the leading reason for the procedure, which can substantially improve an individual’s quality of life.19 Hip replacements are an important indicator of the prevalence of osteoarthritis in a population.
Discussion On US Healthcare
The United States spends more on health care than any other high-income country. The nation often performs worse on measures of health and health care. For the U.S., a first step to improvement is ensuring that everyone has access to affordable care. Not only is the U.S. the only country we studied not having universal health coverage, its health system appears to be designed to discourage people from using services.
Affordability remains the top reason why some Americans do not sign up for health coverage. High out-of-pocket costs cause nearly half of working-age adults to skip or delay getting needed care.20 The Inflation Reduction Act will help reduce the high cost of certain drugs and cap out-of-pocket costs for older Americans. It is a step in the right direction.21 But it will take much more to make health care as easy to access as it is in other high-income countries.
A second step is containing costs. Other countries have achieved better health outcomes while spending much less on health care overall. In the U.S., high prices for health services continue to be the primary driver of this elevated spending.22 Policymakers and health systems could look to some of the approaches taken by other nations to contain overall health spending, including the care and the administrative costs.
A third step is better prevention and management of chronic conditions. Critical to this is developing the capacity to offer comprehensive, continuous, well-coordinated care. Decades of underinvestment, along with an inadequate supply of health care providers, have limited American access to effective primary care.23
The findings of our international comparison demonstrate the importance of a health care system supporting chronic disease prevention and management. Much less, the early diagnosis and treatment of medical problems, affordable access to health care coverage, and cost containment. All are among the key functions of a high-performing system. Since other countries have found ways to do these things well, the U.S. could also.