This is quite a bit of band width to be recited at Angry Bear. The problem with healthcare facing smaller hospitals and healthcare is the lack of resource once you are outside of the metropolitan areas. You are pretty much on your own. If the resource is not there, it may be an hour or so away. Can treatment wait that long? It is something to think about. Saving Rural Hospitals – Problems and Solutions for Rural Hospitals, chqpr.org. I broke this report into two and maybe three, or even more parts. This information people do not know about, have not read about or do not care about in living their lives today. Overall the importance of providing healthcare nationwide is important. The Importance of Rural Hospitals There are two very
Topics:
Bill Haskell considers the following as important: Healthcare, Rural Hospitals
This could be interesting, too:
Bill Haskell writes Families Struggle Paying for Child Care While Working
Joel Eissenberg writes RFK Jr. blames the victims
Joel Eissenberg writes The branding of Medicaid
Bill Haskell writes Why Healthcare Costs So Much . . .
This is quite a bit of band width to be recited at Angry Bear. The problem with healthcare facing smaller hospitals and healthcare is the lack of resource once you are outside of the metropolitan areas. You are pretty much on your own. If the resource is not there, it may be an hour or so away. Can treatment wait that long? It is something to think about.
Saving Rural Hospitals – Problems and Solutions for Rural Hospitals, chqpr.org.
I broke this report into two and maybe three, or even more parts. This information people do not know about, have not read about or do not care about in living their lives today. Overall the importance of providing healthcare nationwide is important.
The Importance of Rural Hospitals
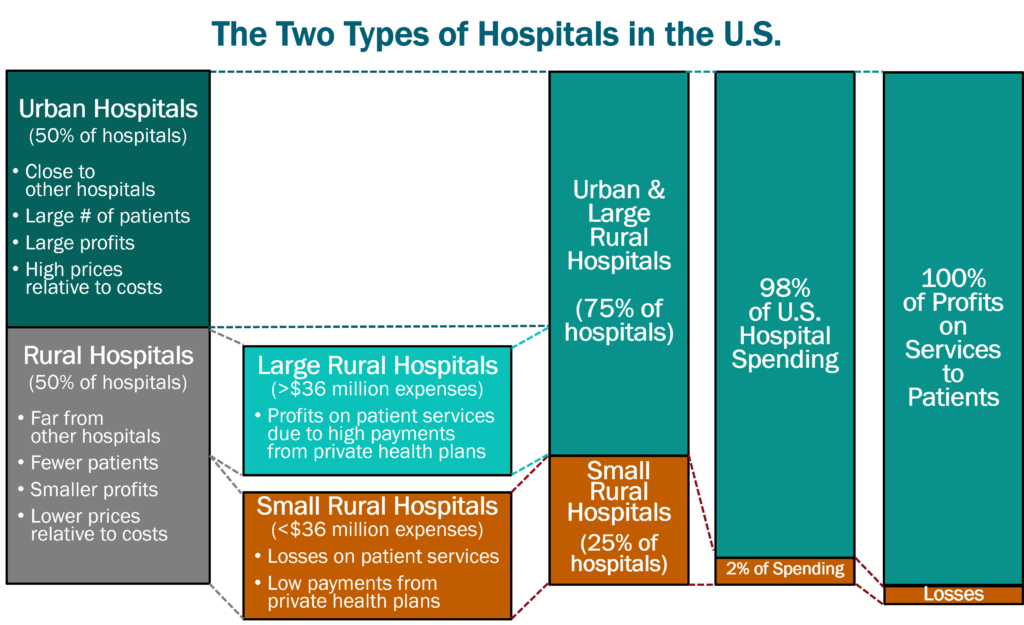
There are two very different types of hospitals in the U.S: (1) small rural hospitals, and (2) urban and large rural hospitals. There are over 1,000 small rural hospitals1, representing nearly one-fourth of all the short-term general hospitals in the country, but they receive only 2% of total national hospital spending.
Small rural hospitals provide most or all of the healthcare services in the small communities they serve. Small rural hospitals deliver not only traditional hospital services such as emergency care, inpatient care, and laboratory testing. Most of them also deliver primary care and inpatient rehabilitation services. The majority of the communities they serve are at least a half-hour drive from the nearest alternative hospital, and many communities have no alternate sources of health care.
The services provided by small rural hospitals are also important for residents of urban areas. Most of the nation’s food supply and energy production comes from rural communities. Farms, ranches, mines, drilling sites, wind farms, and solar energy facilities cannot function without an adequate, healthy workforce. People are less likely to live or work in rural communities not having an emergency department and other healthcare services. Many popular recreation, historical, and tourist sites are located in rural areas. Visitors to those sites need access to emergency services if they have an accident or medical emergency.
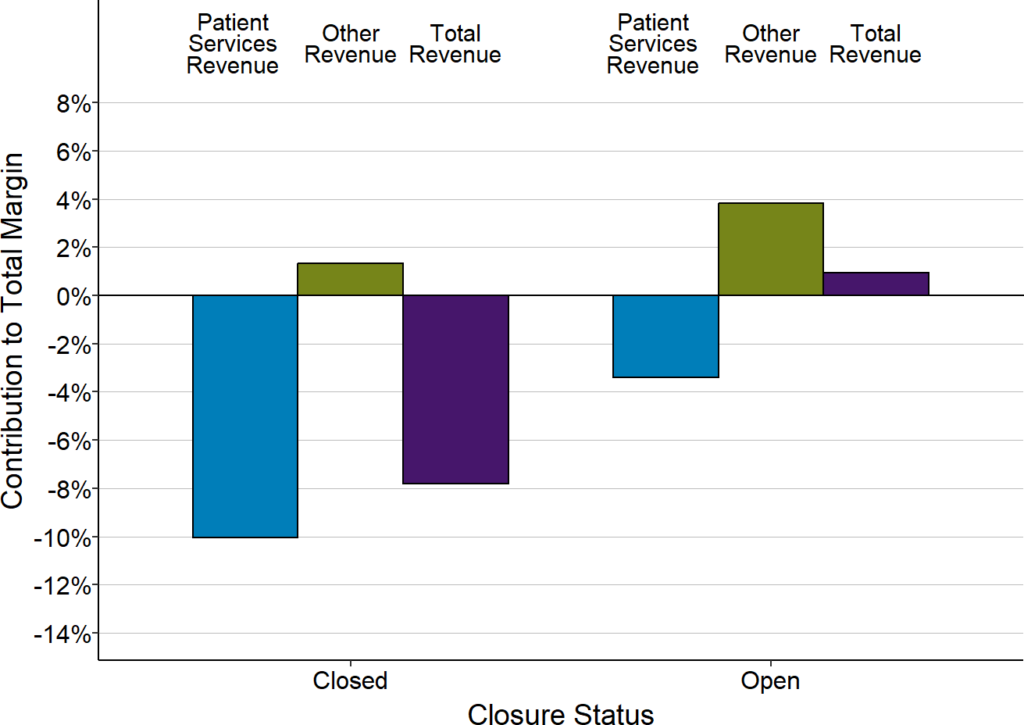
The Crisis Facing Rural Healthcare
Small rural hospitals are struggling to survive and rural communities are being harmed. The majority of small rural hospitals are losing money delivering patient services. More than 100 rural hospitals have closed in the past decade, and most of these were small rural hospitals. In most cases, the closure of the hospital resulted in the loss of both the emergency department and other outpatient services, and residents of the community must now travel much farther when they have an emergency or need other healthcare services. This increases the risk of death or disability when accidents or serious medical conditions occur, but it also increases the risk of health problems going undiagnosed or inadequately treated due to lack of access to care.
More than 600 rural hospitals – over 30% of all rural hospitals in the country – are at risk of closing in the near future, and over 300 of these hospitals are at immediate risk of closing. Most of the at-risk hospitals are small rural hospitals located in isolated communities where loss of the hospital will severely limit access to health care services. Millions of people could be directly harmed if these hospitals close, and people in all parts of the country could be affected through the impacts on workers in agriculture and other industries.
The Causes of the Financial Problems at Small Rural Hospitals
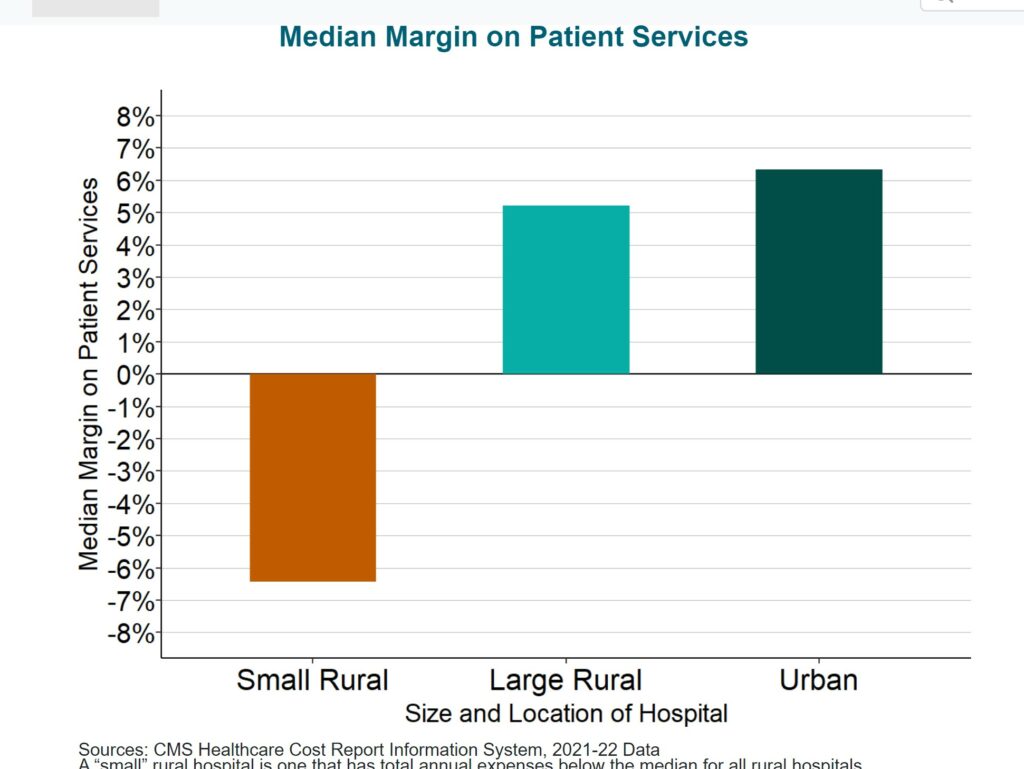
Small rural hospitals are being forced to close because of not being paid enough to cover the cost of delivering care to patients in rural areas. Most small rural hospitals lose money delivering services to patients, while most urban hospitals and larger rural hospitals make profits on patient services.
Contributions of Patient Services and Other Revenues
to Total Margins at Closed and Open Small Rural Hospitals
Each bar represents the median value for rural hospitals that (1) have closed since 2015 or (2) remained open in 2022. Only rural hospitals with less than $38 million in expenses are included. The value for each hospital is the median for the three years prior to closure (for hospitals that had closed) or the median for the three years prior to 2020 (for hospitals that were open in 2022) of (a) the dollar margin (i.e., profit or loss) earned on services to patients, (b) the amount of revenue received from sources other than patient services, or (c) the total hospital revenue, divided by the hospital’s total expenses. This shows how much revenue from patient services and other sources of revenue contributed to the hospital’s total margin.
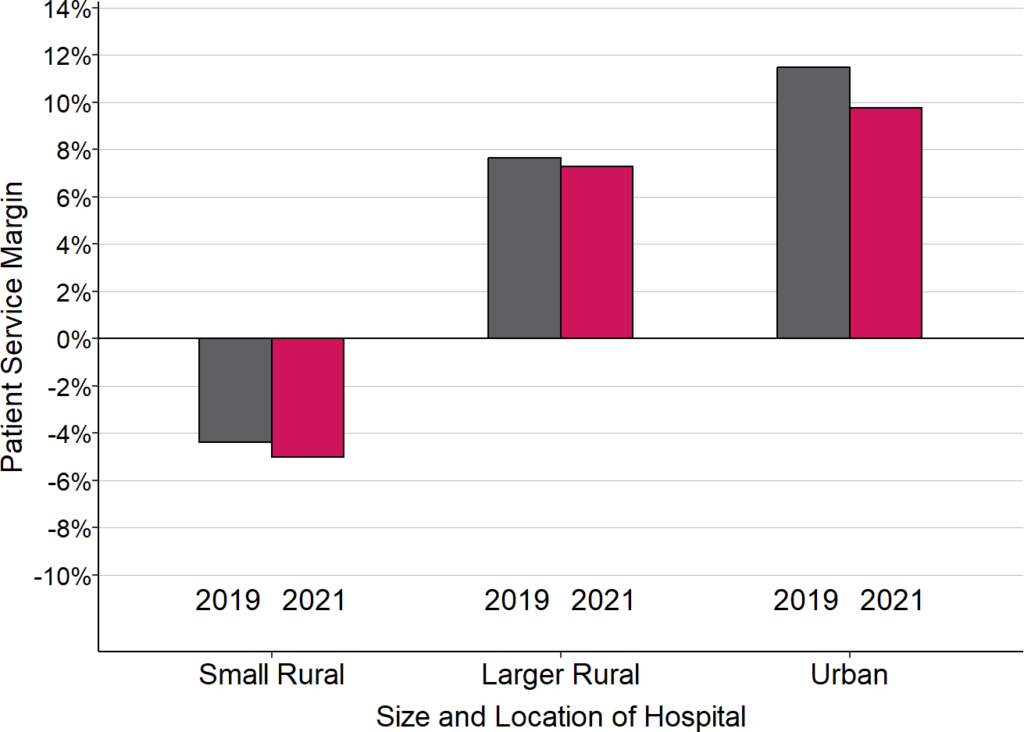
The Impact of the Pandemic on Rural Hospitals
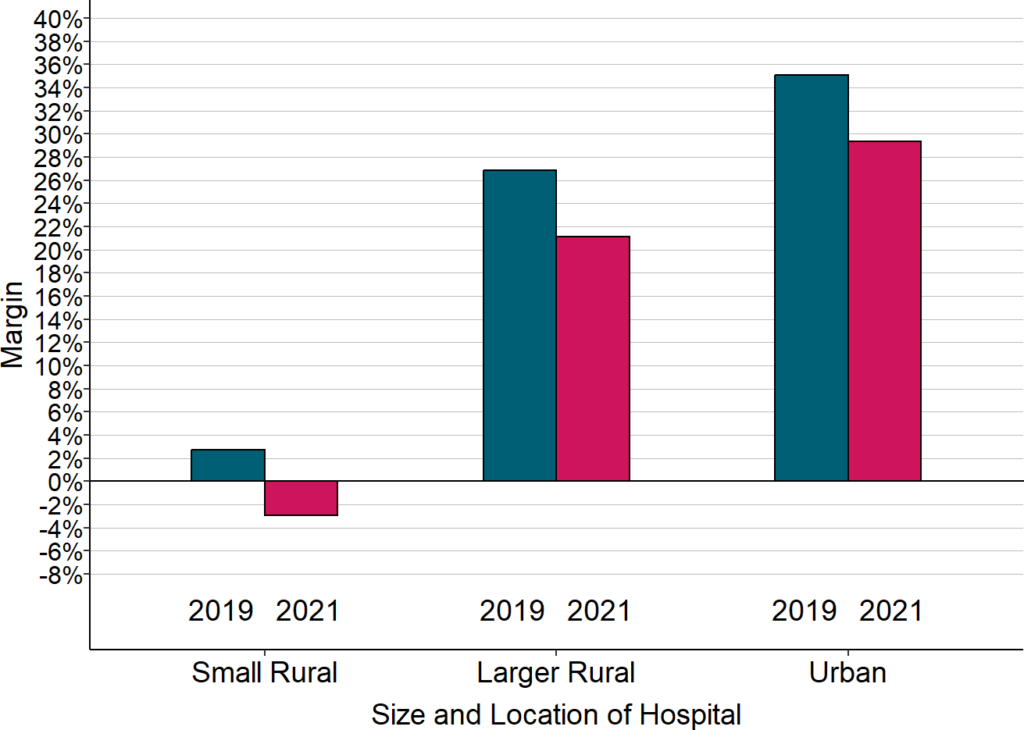
Small rural hospitals had greater losses on patient services during the pandemic. Most rural hospitals experienced lower margins on patient services during the pandemic. Since a majority were losing money on patient services prior to the pandemic, the reductions in margins during the pandemic pushed them even further into the red. In contrast, even though larger rural hospitals and urban hospitals also experienced lower margins, most of them continued to generate profits on patient services overall.
Change in Median Margins on Patient Services
“Small Rural” hospitals are rural hospitals with annual expenses less than the median for all rural hospitals. 2020 is defined here as the hospital’s fiscal year including the March-June 2020 period. 2021 is the year that followed 2020, and 2019 is the year that preceded it.
The primary reason overall patient service margins at rural hospitals decreased during the pandemic was higher losses on patients insured by private health plans (including Medicare Advantage plans). The losses on patients insured by private health plans hurt the smallest rural hospitals the most because they were already receiving low payments from private payers prior to the pandemic. Although hospitals of all sizes experienced lower margins during the pandemic on services to patients with private health insurance, the reductions meant that most small rural hospitals lost money providing services to these patients.
Median Margin on Patients With Private Insurance
“Small Rural” hospitals are rural hospitals with annual expenses less than the median for all rural hospitals. 2020 is defined here as the hospital’s fiscal year that included the March-June 2020 period. 2021 is the year that followed 2020, and 2019 is the year that preceded it. The margin shown is the difference between the revenues received from private insurance plans (including Medicare Advantage plans) and the cost of the services delivered to the patients insured by those plans, divided by the cost.
Federal assistance enabled small rural hospitals to continue operating during the pandemic, but because assistance has now ended, many hospitals could be forced to close. Despite the higher losses on patient services they experienced, only a few rural hospitals closed during the pandemic because of the special federal funding that was available. Most rural hospitals received significant amounts of federal aid enabling them to continue operating. However, this federal assistance was only temporary. The losses on patient services will likely continue or worsen because of the higher costs rural hospitals are now facing, and without the extra federal assistance, many hospitals will be at risk of closing.
The Problems With Current Payment Methods
Standard payments for hospital services are not large enough to cover the higher cost of delivering services in small rural communities.
AB: This makes sense as similar is experienced in small businesses which do not have the volume. The same holds true for small hospitals.
The average cost of an emergency room visit, inpatient day, laboratory test, imaging study, and primary care visit is inherently higher in small rural hospitals and clinics than at larger hospitals because there is a minimum level of staffing and equipment required to deliver each of these services regardless of how many patients need to use them. For example, a hospital Emergency Department has to have at least one physician available around the clock in order to respond to injuries and medical emergencies quickly and effectively, regardless of how many patients actually visit the ED. A smaller community will have fewer ED visits, but the cost of the ED will be the same, so the average cost per visit will be higher. Consequently, fees that are high enough to cover the average cost per service at larger hospitals will fail to cover the costs of the same services at small hospitals. Many private health plans pay small rural hospitals less than they pay larger hospitals for the same services, even though the cost per service at the smaller hospitals is inherently higher.
Critical Access Hospital status reduces a small rural hospital’s losses only on services to Original Medicare beneficiaries, and it makes services less affordable for the patients. Most small rural hospitals are classified as Critical Access Hospitals, which enables them to receive cost-based payment for patients with Original Medicare and some Medicaid programs. Although this results in higher payments for Original Medicare patients than the hospital would otherwise receive, it does nothing to reduce losses on uninsured patients and losses on those with other types of insurance, including patients with a Medicare Advantage plan. Moreover, Medicare rules require patients to pay higher cost-sharing amounts in order to receive services at Critical Access Hospitals than at other hospitals, so the higher payments for the hospital can have a negative financial impacts on its patients.
Current methods of payment penalize hospitals for efforts to improve the health of rural residents. If community residents are healthier and need fewer ED visits and other services, the hospital’s revenues will decrease, but the cost of maintaining the essential services will not change, thereby increasing financial losses at the hospital. The same problem occurs under Medicare’s cost-based payment system for Critical Access Hospitals because Medicare’s share of the hospital’s costs decreases if Medicare beneficiaries need fewer services.
Next: The Serious Problems With Commonly Proposed Solutions