Another add-on from yesterday as to why people should take precautionary actions when confronted with a pandemic such as Covid-19, the flu, or other contagions. There was much resistance to taking precautionary measures under the guise of a freedom to do what they wish to do mentality. Thousands of people paid with their lives after contracting Covid-19. Many of them decided they did not need to take any precautionary actions. Masks, social distancing and vaccinations worked by Merrill Goozner GoozNews Under U.S. law, states have the primary responsibility for protecting public health. The Centers for Disease Control and Prevention can make recommendations and give grants for specific programs, but the federal government allows state and
Topics:
Angry Bear considers the following as important: COVID-19, Education, Healthcare
This could be interesting, too:
Bill Haskell writes Families Struggle Paying for Child Care While Working
Joel Eissenberg writes RFK Jr. blames the victims
Joel Eissenberg writes The branding of Medicaid
Joel Eissenberg writes The Trump/Vance Administration seeks academic mediocrity
Another add-on from yesterday as to why people should take precautionary actions when confronted with a pandemic such as Covid-19, the flu, or other contagions. There was much resistance to taking precautionary measures under the guise of a freedom to do what they wish to do mentality. Thousands of people paid with their lives after contracting Covid-19. Many of them decided they did not need to take any precautionary actions.
Masks, social distancing and vaccinations worked
by Merrill Goozner
GoozNews
Under U.S. law, states have the primary responsibility for protecting public health. The Centers for Disease Control and Prevention can make recommendations and give grants for specific programs, but the federal government allows state and local health departments to determine their own priorities.
The COVID-19 pandemic exposed the weakness of this decentralized approach. Within a month of then-president Donald Trump declaring a national emergency on March 13, 2020, the CDC (after some initial waffling) recommended everyone wear masks and engage in social distancing when out in public. By November, 37 states had adopted mask mandates or required people stay separated when in public places.
The federal government never officially recommended states adopt stay-at-home policies. But within three months of the outbreak, 42 states had issued such orders for “non-essential” businesses. That spring, over three-quarters of U.S. public schools switched to remote learning, a number that rose to 80% by fall. Many businesses (especially restaurants) shut down or switched to take-out only. For millions of workers with desk jobs, work-at-home became a way of life.
However, enforcement of all those policies was largely non-existent. Widespread resistance emerged within months. Ditto for vaccine mandates once the two-shot regimen became widely available in the fall of 2021.
Resistance began at the top. When, on September 26, 2020, then-president Donald Trump held an outdoor ceremony to announce Amy Coney Barrett’s nomination to the Supreme Court, everyone sat cheek-by-jowl in the Rose Garden. Only a few wore masks. During the first debate on September 29th, Trump mocked Joe Biden: “I don’t wear a mask like him. Every time you see him, he’s got a mask.” A day later, Trump, the First Lady and senior advisor Hope Hicks tested positive for COVID, forcing the president to enter Walter Reed Hospital for a three-day stay.
Numerous businesses that had been deemed non-essential challenged the shut-down orders. Court suits were filed in Wisconsin, Pennsylvania, Arizona and New Mexico. Trump encouraged businesses to stay open saying, “We can’t have a cure that’s worse than the disease.”
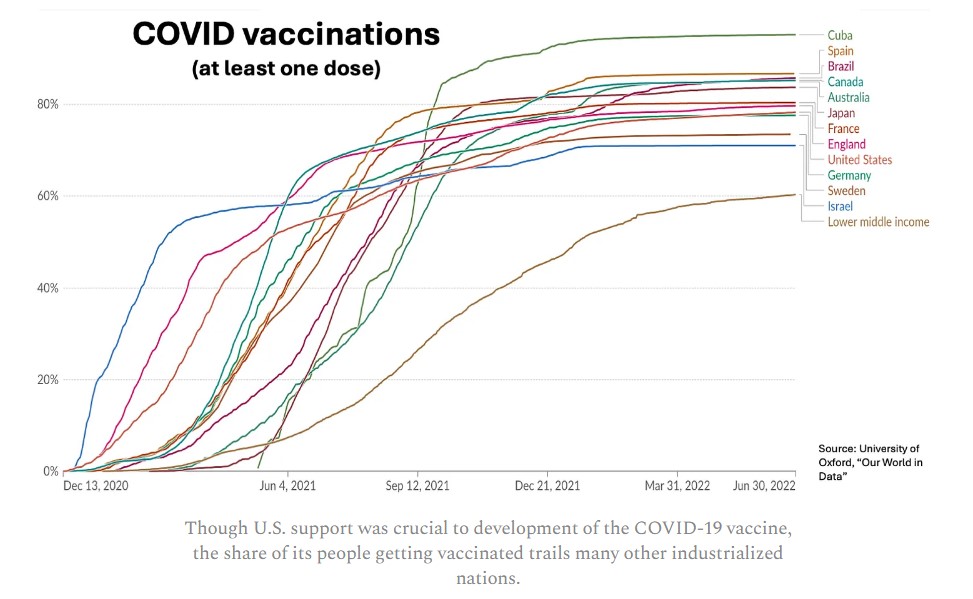
During 2021, after the new COVID-19 vaccine proved remarkably effective at reducing the severity of the disease, President Biden required vaccinations for federal employees and contractors. He proposed all businesses with over 100 employees either do the same or test their employees weekly. Governors in GOP-run states declared the move “terrifying” and a “power grab,” which helped stoke resistance among a small but vocal minority of the population. The U.S. vaccination rate remains in the lower tier among advanced industrial nations.
51 petri dishes worth studying
In other words, the U.S. failed to mount an effective national response to COVID-19. Instead, states and the District of Columbia adopted a patchwork quilt of requirements and recommendations. Even where restrictions and mandates were in place, enforcement was mostly a non-event with states relying on voluntary compliance.
Still, some of those measures may have had a huge impact on reducing disease incidence and mortality during the pandemic. Given the uneven nature of their adoption between states, the U.S. became the ideal place for studying the impact of various interventions.
The challenge was taken up by Christopher Ruhm, a professor of public policy and economics at the University of Virginia. Ruhm’s study, released today on the JAMA Health Forum website, shows states that adopted the strictest COVID-protection policies had significantly lower death rates than states that had the least restrictive policies. He calculates that if every state had adopted the policies enacted by the ten most restrictive states, anywhere from 118,000 to 148,000 additional lives would have been saved between July 2020 and June 2022, a period when the pandemic was raging in almost every state in the nation.
On the other hand, if every state had followed the path taken by the ten least restrictive states – a move pushed by conservative scholars associated with the Great Barrington Declaration, which encouraged the pursuit of “herd immunity” to curb COVID – an additional 150,000 to 200,000 lives would have been lost. There was an estimated 25% to 48% difference in mortality rates between the most restrictive and least restrictive states.
“Strong COVID-19 restrictions saved lives,” Ruhm concluded. “The death toll was probably considerably higher than it would otherwise have been in states that resisted imposing these restrictions, banned their use, or implemented them for only relatively short periods of time.”
Ruhm, who served as a senior economist for the Council on Economic Advisers during the Clinton administration, excluded data from the first four months of the pandemic. During that initial phase, half of all COVID cases and deaths took place in just four northeastern states with the most exposure to foreign travelers. In addition, intervention measures in most states were just ramping up as the scientific understanding of how the disease spread evolved.
The study evaluated the effects of 10 separate restrictions and individual behaviors enacted in that first year. The restrictions included requirements and/or restrictions for both masking and vaccinations; self-reported masking adherence; stay-at-home orders; closures of restaurants, bars, theaters, schools and other leisure time activities; and restrictions on public gatherings.
Most v. least restrictive states
Ruhm created a composite score for each state and then ranked them from “most restrictive” to “least restrictive.” The ten states with the most restrictive policies were (in alphabetical order): California, Connecticut, the District of Columbia, Delaware, Hawaii, Illinois, New Mexico, New York, Oregon and Washington. The ten states with the least restrictive policies were Florida, Georgia, Idaho, Iowa, Oklahoma, South Carolina, South Dakota, Tennessee, Texas and Utah.
He then compared the all-cause mortality rates in those two groups to their pre-COVID rates. Overall, the difference between the two groups was stark. But not all interventions were equally effective. And some weren’t effective at all.
For instance, states that adopted the strictest policies on masking and social distancing saw the smallest rise in all-cause mortality during the pandemic. States that resisted those policies had the biggest increases. Vaccine mandates were also highly effective in reducing death rates as would be expected given the vaccine’s effectiveness in reducing disease severity.
Picture
Though U.S. support was crucial to development of the COVID-19 vaccine, the share of its people getting vaccinated trails many other industrialized nations.
Major limitations on social, business and school activities, on the other hand, did not reduce the death rates. But neither did they raise them, a claim that has been made by some opponents of restrictions who suggest limits on access to health care, among other things, cost lives.
In an interview this week, Ruhm told me that some of the study’s peer reviewers questioned that finding. He wishes everyone would lower their defenses and begin learning from the experience of the past four years, which is now possible if we take a close look at the data.
Some things worked very well; others not so well, he said. “It is clear schools were closed for too long in many places. The costs of that exceeded any benefit. But what is even more frustrating is this notion that overall these restrictions did not work.
“Vaccinations were incredibly important as were masks and social distancing. Maybe we should have realized faster than some (restrictions) were not ideal. There were cases where the balance should have been tilted in different ways. But this notion that these things were just harmful or ineffective? An objective look at the evidence does not support that view. As packages, the states that had stronger restrictions saved hundreds of thousands of lives.”
The next Congress needs to make pandemic preparedness one of its highest priorities. A first step would be establishing a commission that can draw firm conclusions about what worked and what didn’t during the COVID-19 pandemic. It must address flaws in our decentralized response system. And it should provide guidance on what it will take to win broad public acceptance for necessary public health measures, which will save lives during the next pandemic, an inevitability in our warming world.