Center for Healthcare Quality and Payment Reform CHQPR I started reviewing rural hospitals a little over a year ago. Not much has changed. These smaller hospitals lack for resource and manpower because of their budget restraints. Services they provide may not be covered by a patient’s fees. As a result, they are always battling their budget. If they are a part of the 340B program and close to a city, larger hospitals may buy them out and take the benefit of the 340B. What remains is a shell of the former hospital. The following post is a brief rundown of what is need by these small hospitals. More later over the weeks. Saving Rural Hospitals – Problems and Solutions for Rural Hospitals (chqpr.org) A good payment system for rural hospitals
Topics:
Angry Bear considers the following as important: Healthcare, US EConomics
This could be interesting, too:
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Bill Haskell writes The North American Automobile Industry Waits for Trump and the Gov. to Act
Bill Haskell writes Families Struggle Paying for Child Care While Working
Joel Eissenberg writes Time for Senate Dems to stand up against Trump/Musk
Center for Healthcare Quality and Payment Reform CHQPR
I started reviewing rural hospitals a little over a year ago. Not much has changed. These smaller hospitals lack for resource and manpower because of their budget restraints. Services they provide may not be covered by a patient’s fees. As a result, they are always battling their budget. If they are a part of the 340B program and close to a city, larger hospitals may buy them out and take the benefit of the 340B. What remains is a shell of the former hospital.
The following post is a brief rundown of what is need by these small hospitals. More later over the weeks.
Saving Rural Hospitals – Problems and Solutions for Rural Hospitals (chqpr.org)
A good payment system for rural hospitals must achieve three key goals:
- Ensure availability of essential services in the community;
- Enable timely delivery of the services patients need; and
- Support delivery of appropriate, high quality, affordable care.
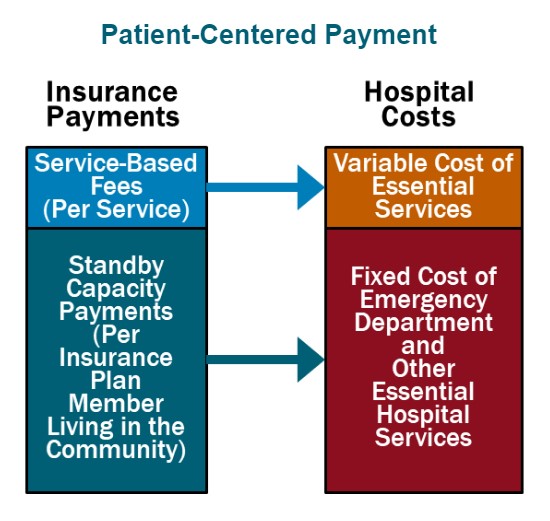
Patient-Centered Payment for rural hospitals can achieve all three goals through the following four components:
- Standby Capacity Payments to Support the Fixed Costs of Essential Services. Each health insurance plan (Medicare, Medicaid, Medicare Advantage, and commercial insurance) should pay a Standby Capacity Payment to the rural hospital based on the number of members of that plan who live in the community (regardless of the number of services the patients receive). This ensures that the hospital has adequate revenues to support the minimum standby costs of essential services such as the emergency department, inpatient unit, and laboratory.
- Service-Based Fees for Diagnostic and Treatment Services Based on Variable Costs. Rural hospitals should continue to receive payments from health plans for delivering individual services, but under Patient-Centered Payment, the Service-Based Fees could be much lower than current payments. Since the hospital would receive Standby Capacity Payments to support the fixed costs of essential services, the Service-Based Fees would only need to cover the additional costs incurred when additional services are delivered. This means that if patients stay healthy and need fewer services, the hospital’s revenues and costs will decrease by similar amounts, so the hospital’s margin will not be harmed.
- Accountability for Quality and Spending. In return for receiving adequate payments to support essential services, rural hospitals should take accountability for delivering evidence-based services safely and efficiently.
- Value-Based Cost-Sharing for Patients. TThe amount that a patient has to pay out of pocket to receive necessary services should be affordable for the patient, so patients are not prevented from obtaining the care needed to improve their health.
In addition, rural hospitals that operate Rural Health Clinics or primary care practices need to be paid for primary care services using Patient-Centered Primary Care Payment. The clinic/practice should receive monthly Wellness Care Payments and Chronic Condition Management Payments to support proactive preventive care and chronic disease care delivered by primary care teams, rather than being paid only for office visits with physicians/clinicians, as well as Acute Care Visit Fees when patients experience a new symptom or problem. The payments should provide the clinic/practice with adequate resources and flexibility to help patients stay as healthy as possible and to deliver timely, evidence-based care when the patients experience health problems.
This is a patient-centered approach to payment because it is designed to support the services that patients need, not to increase profits for either hospitals or health insurance plans. Patient-Centered Payment would provide adequate funding to support services in small rural communities without the kinds of problematic incentives to deliver unnecessary services or to stint on care that exist in current payment systems and “value-based” payments.
How to Save Rural Hospitals and Strengthen Rural Healthcare
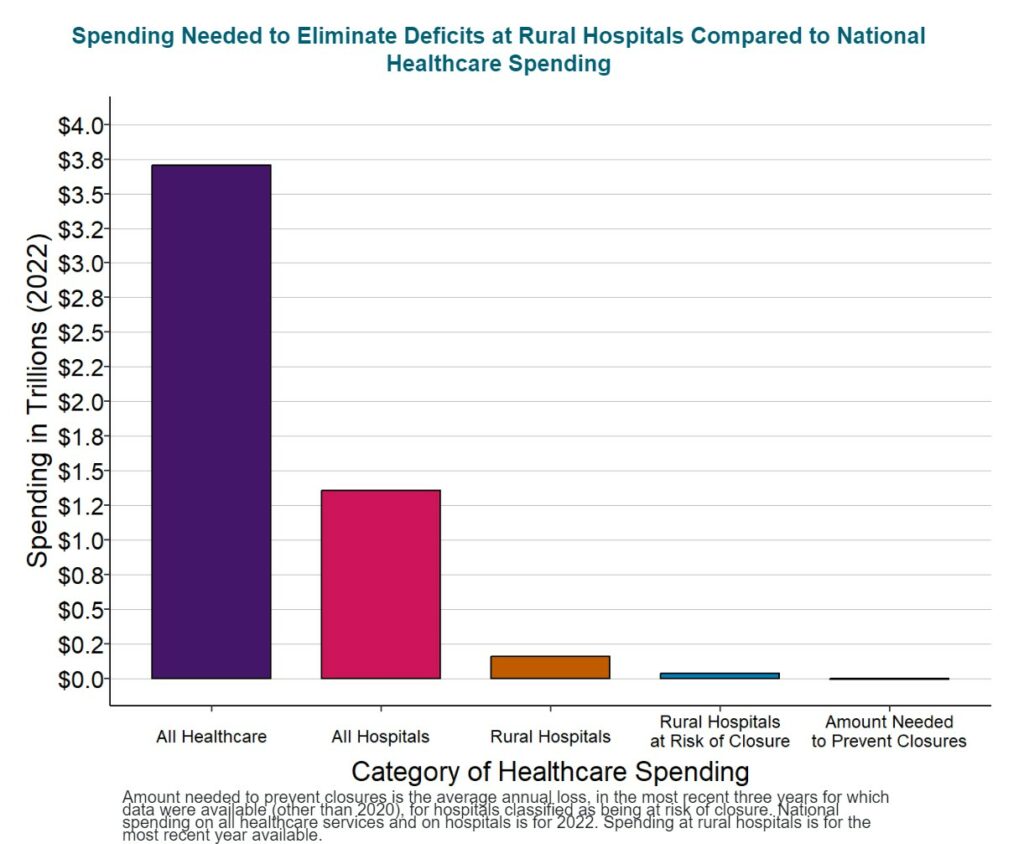
It will cost about $4 billion per year to prevent closures of the at-risk hospitals and preserve access to rural healthcare services, an amount equal to only 1/10 of 1% of total national healthcare spending. No payment system will sustain rural hospitals and clinics unless the amounts of payment are large enough to cover the cost of delivering high-quality care in small rural communities. Because current payments are below the costs of delivering services, an increase in spending by all payers will be needed to keep rural hospitals solvent, but $4 billion is a tiny amount in comparison to the more than $3.3 trillion currently spent on healthcare and the more than $1.3 trillion spent on all urban and rural hospitals in the country. Moreover, most of the increase in spending will support primary care and emergency care, since these are the services at small rural hospitals where the biggest shortfalls in current payments exist.
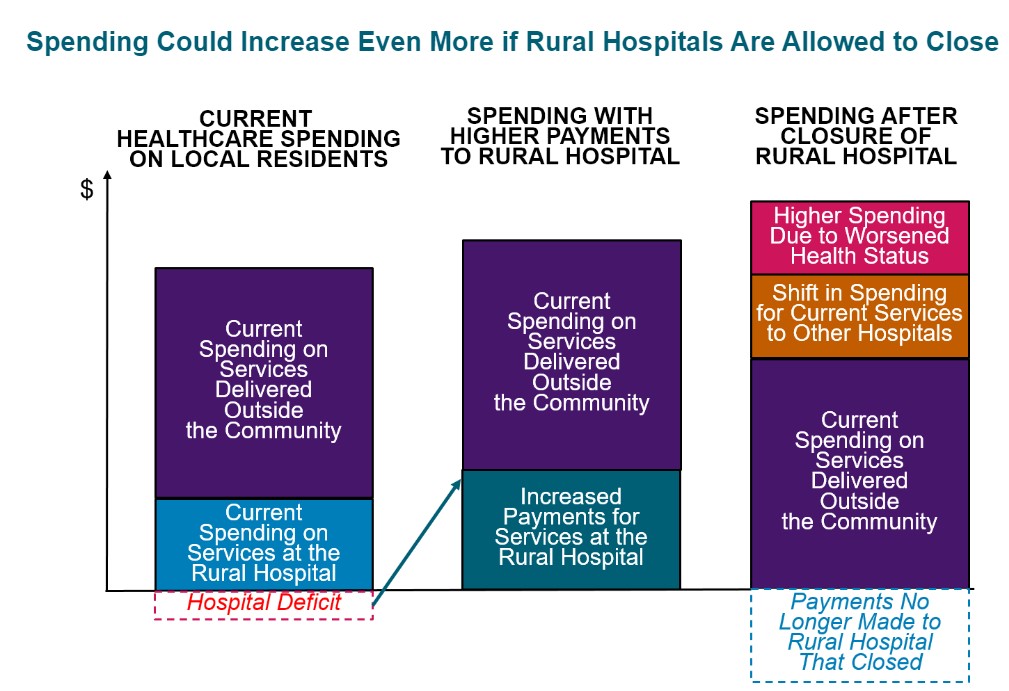
Spending would likely increase even if the hospitals close. The reduced access to preventive care and delays in treatment resulting from a rural hospital closure will cause residents of the community to need even more services in the future. Paying more now to preserve local healthcare services is a better way to invest resources.
Citizens, businesses, local governments, state government, and the federal government must all take action to ensure that every payer provides adequate and appropriate payments for small rural hospitals and clinics:
- Businesses, state and local governments, and rural residents must demand that private health insurance companies change the way they pay small rural hospitals. The biggest cause of negative margins in most small rural hospitals in most states is low payments from private insurance plans and Medicare Advantage plans. Private insurance companies are unlikely to increase or change their payments unless businesses, state and local governments, and residents choose health plans based on whether they pay the local hospital adequately and appropriately.
- State Medicaid programs and managed care organizations need to pay small rural hospitals adequately and appropriately for their services. Expanded eligibility for Medicaid will help more rural residents afford healthcare services, but small rural hospitals cannot deliver the services patients need if Medicaid payments are too low. CMS should authorize states to require Medicaid MCOs to use Patient-Centered Payments and to pay adequately for services at small rural hospitals.
- Congress should create a Patient-Centered Payment program in Medicare for small rural hospitals. Although Medicare is not the primary cause of deficits at small rural hospitals, Medicare needs to pay rural hospitals and clinics in a way that will better sustain services in the long run.
Rural hospitals need to be transparent about their costs, efficiency, and quality, and they should do what they can to control healthcare spending for local residents.
In order to support higher and better payments for hospitals, purchasers and patients in rural communities need to have confidence the hospitals will use the payments to deliver high-quality services at the lowest possible cost. That the hospitals will proactively identify and pursue opportunities to control healthcare costs for community residents. Small rural hospitals should estimate the minimum feasible costs for delivering essential services using an objective methodology. They should proactively work to improve the efficiency of their services, and they should publicly report on the quality of their care.
- A “rural” hospital is a hospital located in an area that is classified as rural by the Health Resources and Services Administration. A “small” rural hospital is one that has total annual expenses below the median for all rural hospitals ($40 million in 2022).
Saving Rural Hospitals, The Crisis in Rural Health Care (chqpr.org)