This is one of the types of care where the resource may not be used as often in rural areas when compared to more populated areas. It is still needed in rural areas. The problem being, how do you get the patient and the baby to a fully equipped hospital an hour or more away. In 2019, I wrote “A Woman’s Right to Safe Healthcare Outcomes,” Angry Bear.” I was asked to write this by women who wanted a man’s perspective. I wrote about clinical trials including women, Essure, and the pregnancy of Lauren Bloomstein. Lauren died after childbirth in an excellent hospital. She had good care. The doctor missed the signs. Issues with giving birth can still occur. Imagine when there is no doctor around to deliver a bay and the nearest facility is on 1+hours
Topics:
Bill Haskell considers the following as important: Healthcare, Hot Topics, Rural Hospitals, US EConomics
This could be interesting, too:
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Joel Eissenberg writes No Invading Allies Act
Bill Haskell writes The North American Automobile Industry Waits for Trump and the Gov. to Act
Bill Haskell writes Families Struggle Paying for Child Care While Working
This is one of the types of care where the resource may not be used as often in rural areas when compared to more populated areas. It is still needed in rural areas. The problem being, how do you get the patient and the baby to a fully equipped hospital an hour or more away. In 2019, I wrote “A Woman’s Right to Safe Healthcare Outcomes,” Angry Bear.” I was asked to write this by women who wanted a man’s perspective. I wrote about clinical trials including women, Essure, and the pregnancy of Lauren Bloomstein. Lauren died after childbirth in an excellent hospital. She had good care. The doctor missed the signs.
Issues with giving birth can still occur. Imagine when there is no doctor around to deliver a bay and the nearest facility is on 1+hours away. This is what the rural hospital situation is like. It is a situation arural hospital must be prepared for and staffed.
This is a copy and paste. I hope other sites post it also.
A Crisis in Rural Maternity Care in the United States
Most Rural Hospitals in the U.S. No Longer Deliver Babies
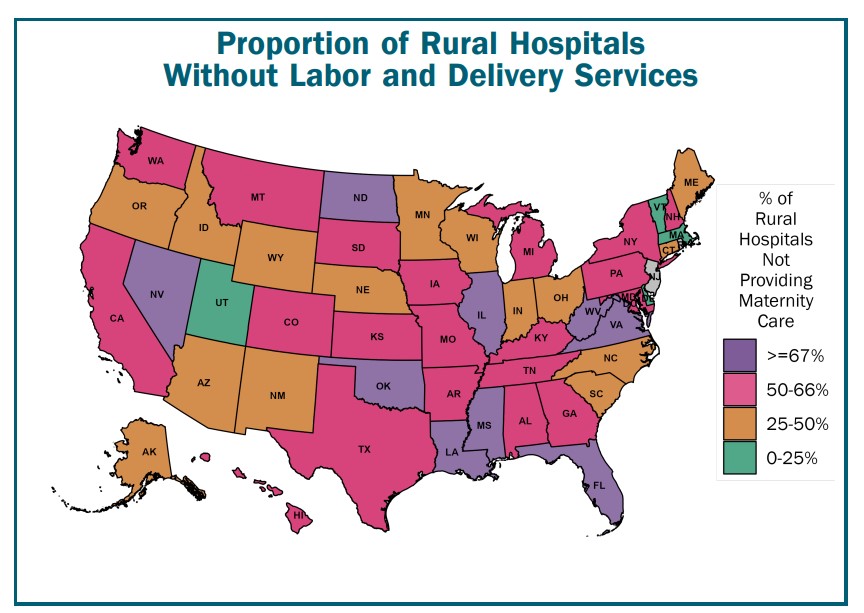
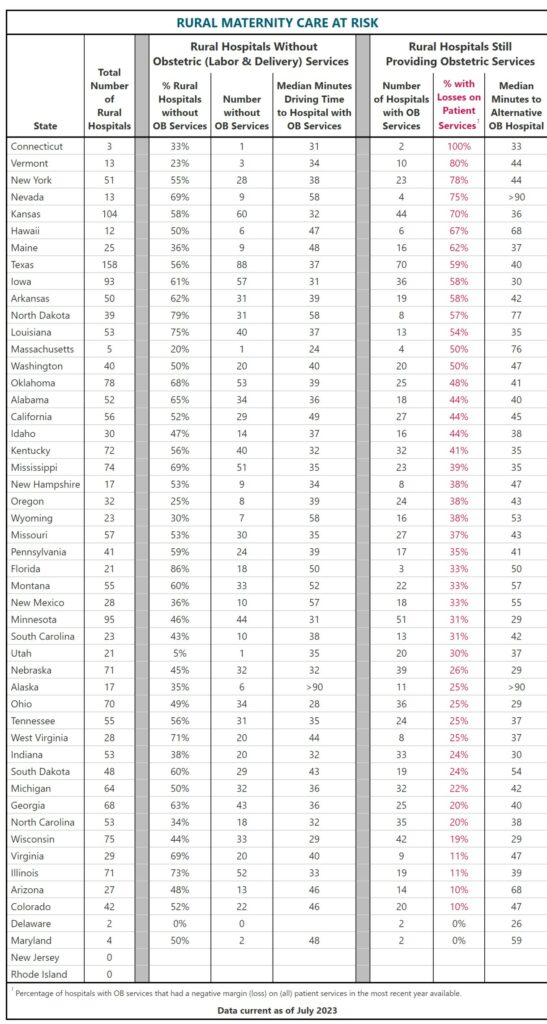
Fewer than half (45%) of the rural hospitals in the U.S. currently offer labor and delivery services, and in 9 states, less than one third do. Over the past decade, more than 200 rural hospitals across the country have stopped delivering babies.
Maternity Care is Far Away for Mothers in Many Rural Communities
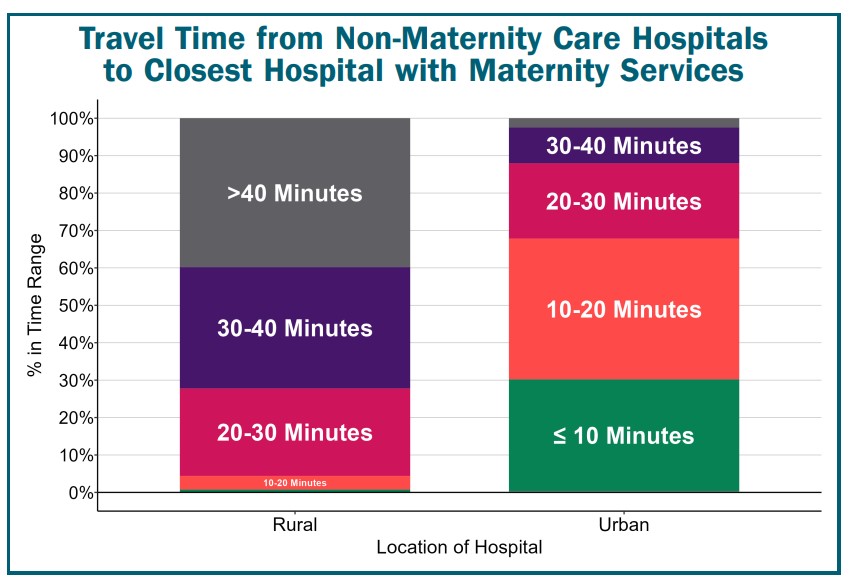
If the closest hospital does not offer labor and delivery services, a pregnant woman may have to travel to a different community to deliver her baby. In most urban areas, the travel time to a hospital with labor and delivery services is under 20 minutes, but in rural areas, the travel time is likely to be at least 30 minutes, and it is often 40 minutes or more. There is a higher risk of complications and death for both mothers and babies in communities that do not have local maternity care services. Women are less likely to obtain adequate prenatal and postpartum care when it is not available locally.
Many More Rural Communities Are at Risk of Losing Maternity Care
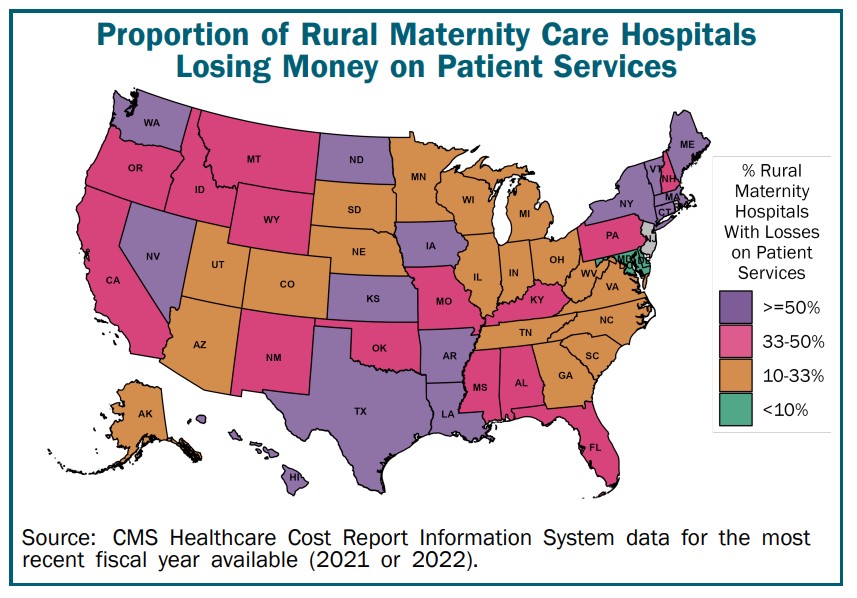
Hundreds of additional communities are at risk of losing maternity care because of the financial challenges rural hospitals are facing. Rural hospitals typically lose money on obstetric care, so if a hospital can’t make enough money on other services to offset those losses, it may be forced to eliminate maternity care in an effort to keep the hospital from closing entirely. More than 1/3 of the rural hospitals that still have labor & delivery services have been losing money on patient services, so their ability to continue delivering maternity care is at risk.
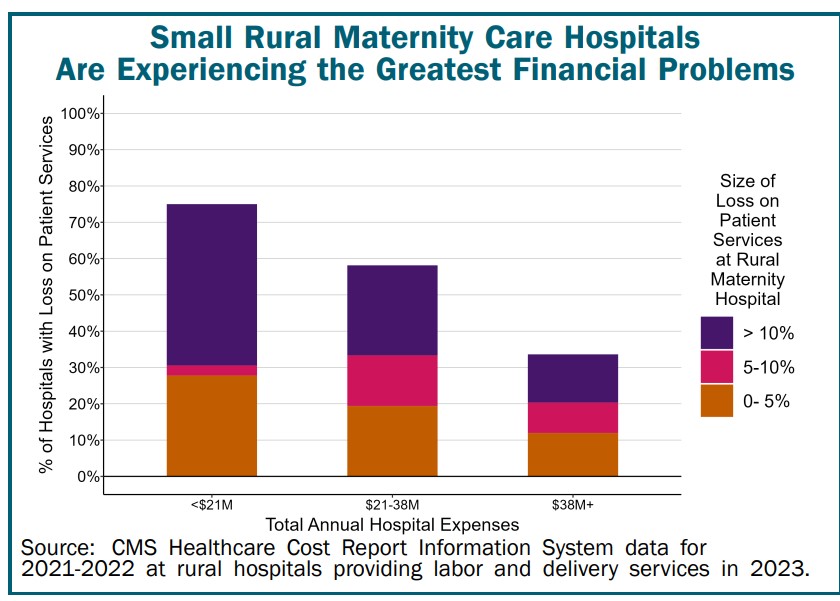
Small Communities Are Most at Risk
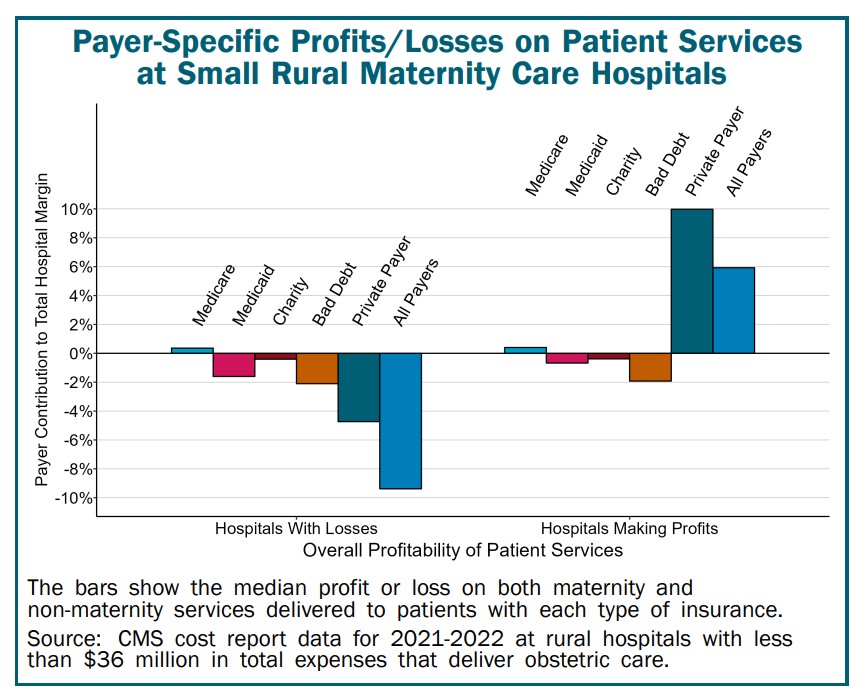
Smaller rural hospitals are more likely to be losing money on patient care services than larger hospitals, and they are more likely to experience large losses. More than half of small rural maternity care hospitals lost money in 2021-22. In most cases, if these hospitals are forced to eliminate maternity care, community residents would have to travel more than 40 minutes to reach a hospital with obstetric services.
Rural Hospitals Without Obstetric Services and Still Providing Obstetric Services
Losses Are Due to Inadequate Payments from Private Payers
As shown to the left, the primary reason small rural maternity care hospitals are losing money is that private insurance plans pay them less than what it costs to deliver many types of services to patients, not just maternity care. Although the hospitals are also losing money on uninsured patients and Medicaid patients, the losses from private payers have the biggest impact on their overall profit margins. Conversely, small rural maternity hospitals that avoid losses are able to do so because their payments from private health plans not only cover the costs of services (of all types) to the patients with private insurance but also offset the hospitals’ losses on services to uninsured and Medicaid patients.
Actions Needed to Preserve and Strengthen Rural Maternity Care
Significant changes in payments from both private and public payers are needed to resolve the financial problems facing rural hospitals before even more maternity care services are lost.
Require That Health Insurance Payments Cover the Actual Cost of Rural Maternity Care
A hospital cannot provide maternity care for its community if private health plans and state Medicaid programs do not pay enough to cover the cost of the services. It is often assumed that low Medicaid payments and uninsured patients are the reasons hospitals lose money on maternity services, but over 40% of births in rural communities are paid for by private health plans, so inadequate payments from private payers also threaten the viability of rural maternity care. Health plans should be required to pay amounts that cover the cost of:
(1) perinatal care services from physicians and midwives;
(2) assistance during labor and delivery from appropriately trained nurses;
(3) anesthesia services (such as when C-Sections are needed); and
(4) telemedicine assistance from specialists for complex cases.
Payment amounts must be higher in communities that have difficulty attracting staff, and payments must also be higher in communities with smaller numbers of births to ensure that revenues cover the fixed costs.
In small rural communities, obstetric services will often be delivered by family physicians rather than obstetricians. Since maternity care will only be a portion of the services these physicians provide, health plans must pay adequately for all of the primary care services they deliver, not just for maternity care.
Rural Health Clinics (RHC) can serve as an important way of supporting maternity care as well as primary care services in rural areas. However, Medicare staffing and productivity standards need to be revised so that RHCs are not penalized for hiring family physicians who spend time delivering maternity care. Private insurers should also be required to pay amounts for primary care visits based on the clinic’s costs, just as Medicare does for its patients.
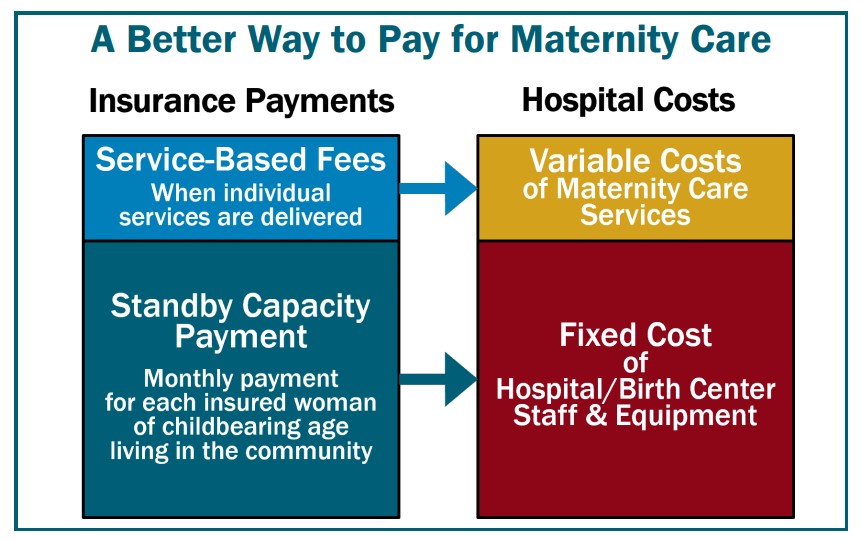
Create Standby Capacity Payments to Support the Fixed Costs of Maternity Care
The financial challenges of delivering maternity care are caused not only by the inadequate amounts paid by insurance plans, but by the problematic method used to pay for services. Currently, a rural hospital is only paid when it actually provides a service. However, a small hospital must be staffed and ready to deliver a baby at all times, even though there will be no deliveries at all on many days.
As a result, when there are fewer pregnancies than expected, the hospital will lose money, even if payments would have been adequate for a larger number of births. A better approach is for private insurers and Medicaid to pay an annual Standby Capacity Payment to the hospital for each insured woman of childbearing age living in the community. This would provide more predictable revenue to cover the fixed costs of maternity care than a purely fee-based system can. The hospital should still receive Service-Based Fees for individual services, but the amounts should be based on the variable costs of the services. More details on this approach are available in A Better Way to Pay Rural Hospitals.
Require Adequate Payments for All Services to Prevent Hospital Closures
Even if payments are adequate to cover the cost of maternity care services, a rural hospital must also receive adequate payments for other essential services, such as its emergency department, or the hospital may not be able to stay open at all. Many small rural hospitals are at risk of closing completely because of the overall financial losses they have been experiencing. Rural Hospitals at Risk of Closing provides more information on this problem and how to address it.