This is an abbreviated version of a Canadian trial which examines whether eliminating out-of-pocket costs would improve the health of people taking the medications by making drugs less costly. The greater impact was amongst lower income participants who may not take drugs as prescribed to lengthen a refill timetable. The elimination of out-of-pocket medication costs resulted in lower and reduced total health spending by a median of 41 and a mean of 65 over 3 years. This suggests the elimination of out-of-pocket medication costs for patients could reduce overall costs of health care. For more detail, please read the full report. Not terribly long and an easy read. JAMA Health Forum – Health Policy, Health Care Reform, Health Affairs, JAMA
Topics:
Bill Haskell considers the following as important: Healthcare, Hot Topics, Out of pocket costs, Pharmaceuticals, reform, US/Global Economics
This could be interesting, too:
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Joel Eissenberg writes No Invading Allies Act
Bill Haskell writes Families Struggle Paying for Child Care While Working
Joel Eissenberg writes How Tesla makes money
This is an abbreviated version of a Canadian trial which examines whether eliminating out-of-pocket costs would improve the health of people taking the medications by making drugs less costly. The greater impact was amongst lower income participants who may not take drugs as prescribed to lengthen a refill timetable. The elimination of out-of-pocket medication costs resulted in lower and reduced total health spending by a median of $1641 and a mean of $4465 over 3 years. This suggests the elimination of out-of-pocket medication costs for patients could reduce overall costs of health care.
For more detail, please read the full report. Not terribly long and an easy read.
JAMA Health Forum – Health Policy, Health Care Reform, Health Affairs, JAMA Network, Nav Persaud, Michael Bedard, and Andrew Boozary.
Objective: The quintuple aim is to reduce costs, improve outcomes, improve patients’ and clinicians’ experiences, and promote health equity.
Health inequities associated with avoidable disparities in outcomes based on income, racism, and other forms of discrimination are estimated to contribute substantially to health spending through poor outcomes for disadvantaged individuals. These inequities can be reduced with better access to basic necessities and health care, including preventive care.
It is thought the elimination of out-of-pocket medication fees on total health care costs addressing cost-related nonadherence has the potential to do so. AB: This would seem logical to me.
Not taking medicines as instructed due to cost, is more prevalent among people with low incomes and is associated with poor health outcomes. Broader prescription drug insurance reduces use of other health care services and has a positive impact on patient outcomes. Coverage gaps or caps on drug insurance generally led to worse outcomes.
The CLEAN Meds (Carefully Selected and Easily Accessible at No Charge Medications) trial examined the effects of free distribution of essential medicines among people experiencing cost-related nonadherence in Ontario, Canada. Physician and hospital care services are universally funded by public payers but do not include prescription medications.
In this (secondary) analysis of the CLEAN Meds trial, a 36-month trial reports the results of free medicine distribution on health care costs and health care encounters among primary care patients experiencing cost-related nonadherence.
Included were adult (≥18 years old) primary care patients who reported cost-related nonadherence (not filling a prescription or not taking as instructed to make a prescription last longer due to the cost) in the 12 months prior to study participation between June 1, 2016, and April 28, 2017. Primary care clinicians identified potentially eligible patients.
A total of 1130 patients were assessed for eligibility, and 786 (mean [SD] age, 51 [14] years; 421 [56.4%] female) were randomly allocated between June 1, 2016, and April 28, 2017. Of those randomized, 39 patients (5.0%) did not consent to the use of health care administrative data, including 13 of 395 patients (3.3%) in the free distribution group and 26 of 391 patients (6.6%) in the usual access group; the characteristics of those included were similar to those in randomized controlled trials. This analysis compared 382 patients in the free distribution group and 365 patients in the usual access group. There were 8 deaths (2.1%) in the free medicine distribution group and 14 deaths (3.8%) in the usual access group (P = .16).
Eliminating out-of-pocket medication fees was associated with a lower median total health care spending over 3 years of $1641 (95% CI, $454-$2792; P = .006.
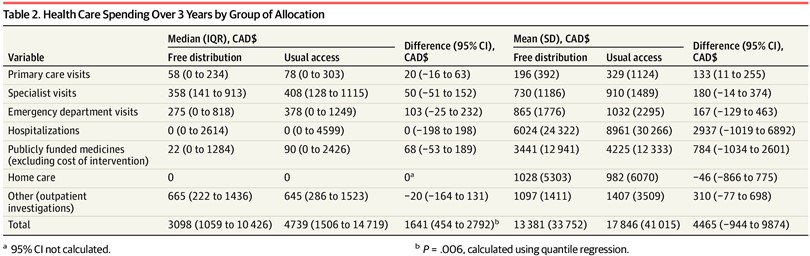
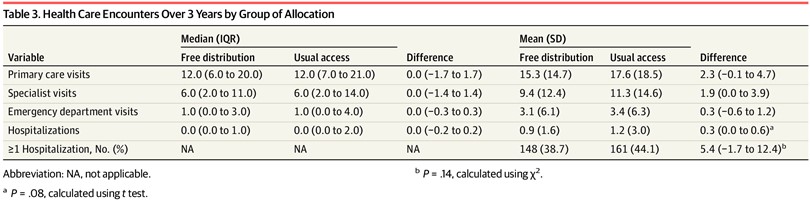
Free distribution was associated with a lower number of participants with very high total health care costs (see Jama Health Form above). Hospitalizations represented the largest cost in both groups (Table 2). Between the free distribution and usual access groups, there was not a statistically significant difference in the number of hospitalizations (mean [SD], 0.9 [1.6] vs 1.2 [3.0]; P = .08) or the rate of being hospitalized at least once (38.7% vs 44.1%; P = .14) (Table 3).
There was no statistically significant reduction in primary care visits, specialist visits, and emergency department visits (Table 3). A relatively small number of participants (10 [2.6%] with free distribution and 17 [4.6%] with usual access) had total health care costs greater than $60 000 (see Jama Health Form above). Mean total costs were $4465 (95% CI, −$944 to $9874) lower over 3 years, or $1488 (95% CI, −$315 to $3291) lower per year.
The findings suggest the promoting of health equity by improving medicine access can reduce overall health care costs. Adding to prior studies showing the free medicine distribution improves the experiences of patients and clinicians. Free medicine distribution may help achieve the quintuple aim that includes both reducing health care spending and improving health equity or fairness in health care and outcomes by ensuring that financial means are not a barrier to realizing the benefits of medicines.