I have long thought that there is a (partially effective) treatment for opiate addiction — suboxone. To review suboxone is a mixture of buprenorphine and naloxone. Buprenorphine is a partial opiate receptor agonist (activator) which also blocks other opiates. At least when taken orally, it relieves opiate craving but does not make people high and prevents them from getting high with other opiates. Naloxone is the well know opiate antagonist used in emergencies. It is not absorbed from the intestine and must be given intravenously or by a nasal spray. In the case of suboxone it is used so that injected suboxone does not cause euphoria, since the buprenorphine is blocked by the naloxone. In contrast if suboxone is taken orally, the naloxone does not
Topics:
Robert Waldmann considers the following as important: history, Hot Topics, suboxone
This could be interesting, too:
NewDealdemocrat writes JOLTS revisions from Yesterday’s Report
Joel Eissenberg writes No Invading Allies Act
Ken Melvin writes A Developed Taste
NewDealdemocrat writes January JOLTS report: monthly increases, but significant downward revisions to 2024
I have long thought that there is a (partially effective) treatment for opiate addiction — suboxone. To review suboxone is a mixture of buprenorphine and naloxone. Buprenorphine is a partial opiate receptor agonist (activator) which also blocks other opiates. At least when taken orally, it relieves opiate craving but does not make people high and prevents them from getting high with other opiates. Naloxone is the well know opiate antagonist used in emergencies. It is not absorbed from the intestine and must be given intravenously or by a nasal spray. In the case of suboxone it is used so that injected suboxone does not cause euphoria, since the buprenorphine is blocked by the naloxone. In contrast if suboxone is taken orally, the naloxone does not prevent the reduction of cravings and the obstruction of opiate receptors by buprenorphine, Sounds to me like a silver bullet.
There are three extreme problems. First most opiate users are not receiving any treatment (this might be because of lack of access or because they choose not to be treated.) “Currently, only about 20% of people with opioid use disorder are getting anything that qualifies as adequate treatment for their disease.” (This is an article by a suboxone advocate, and I think only drug assisted therapy now called MOUD is counted as “anything which qualifies as adequate”. I find the article very convincing. One other important passage is “Myth #4: Suboxone isn’t treatment for addiction if you aren’t getting therapy along with it.
Reality: In a perfect world, addiction treatment should include MOUD as well as therapy, recovery coaching, support groups, housing assistance, and employment support. But that doesn’t mean that one component, in the absence of all of the others, doesn’t constitute valid treatment for addiction.” Note that there is no suggestion that MUAD is the be all and end all of treatment. I have never found any argument against therapy or recovery coaching. By the way, I support them and am extremely non-expert but I have also found no link to evidence that they or support groups reduce drug use or mortality. I am aware of evidence that unconditional housing assistance is followed by reduced drug use.
Importantly until Biden signed the 2023 omnibus spending bill, there were serious bureacratic burdens imposed on physicians before they could prescribe suboxone. The current access to suboxone policy has been in place for less than 2 years.
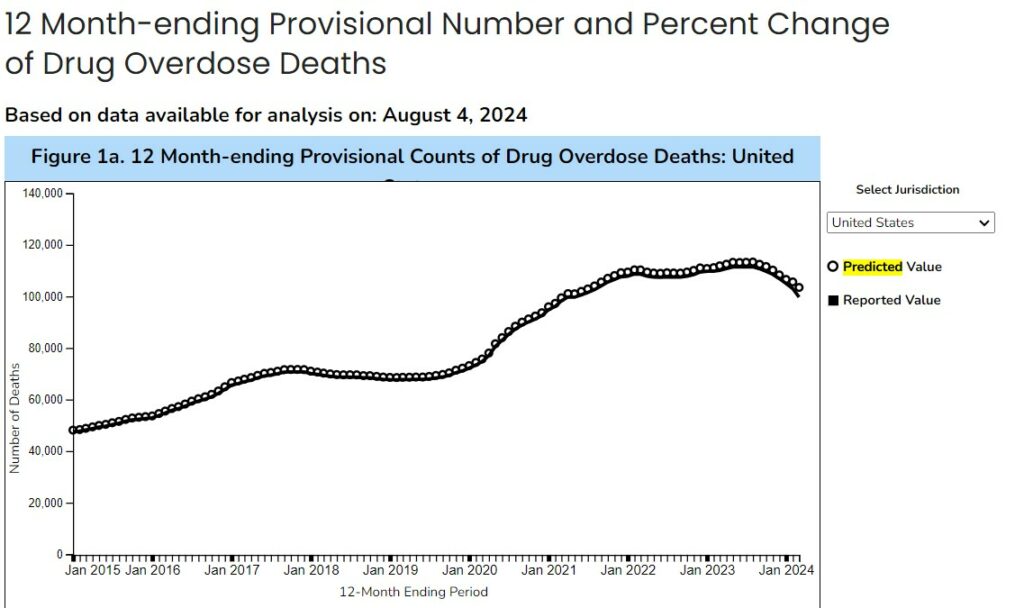
Correlation is not causation (and in this case I am pretty sure we are not seeing causation) but the monthly death rate peaked about then and has declined (oh an explanation “predicted just includes a prediction of the final correction to the provisional count – it is not based on a model which predicts ignoring the omnibus budget act).
Again, I don’t think this is proof or even much in the way of evidence, but it certainly shows that failure of the easy access to suboxone approach has been demonstrated.
This has been, in a way, a long introduction to a Robert is irritated with the New York Times. I argue with :
Rethinking Addiction as a Chronic Brain Disease
Some researchers argue that the roles of social environment and personal choice have to be considered in order to make progress in treating people addicted to drugs.
by Jan Hoffman
I read the arguments
“For decades, medical science has classified addiction as a chronic brain disease . . .
Now, even some in the treatment and scientific communities have been rethinking the label of chronic brain disease.
In July, behavior researchers published a critique of the classification, which they said could be counterproductive for patients and families.
“I don’t think it helps to tell people they are chronically diseased and therefore incapable of change. Then what hope do we have?” said Kirsten E. Smith, an assistant professor of psychiatry and behavioral sciences at Johns Hopkins School of Medicine and a co-author of the paper, published in the journal Psychopharmacology.
“The brain is highly dynamic, as is our environment.”
The recent scientific criticisms are driven by an ominous urgency: “Despite addiction’s longstanding classification as a disease, the deadly public health disaster has only worsened.”
I have the following objections. First “medical science” is defined as the opinions of those officially classified as experts. It would not affect the public health disaster unless and until it is reflected in medical practice. recall the 20% above. The claim is that an approach has been tried and has failed. This claim is demonstrably false.
The claim “therefore incapable of change” is obviously false — many diseases which are considered brain diseases are effectively treated, something which is considered change and which, in other cases, leads to stron advocacy by medical professionals. Kirsten Smith’s claim, or rather rhetorical flourish, is grossly dishonest.
In particular the suboxone advocate above wrote “Use of MOUD has been shown to lower the risk of fatal overdoses by approximately 50%. “If a reduction of disease related mortality of 50% doesn’t count as change, then what does count as change?
Later in the article goes on to quote mainstream drug treatment figures. None argues against counseling etc. Good effects of defining addiction as a disease are noted also by Hoffman. However, the false dichotomy presented in the first paragraphs will remain at least in the minds of those who don’t read whole newspaper articles (that is most readers)